Improved COPD education for better patient outcomes
Posted on November 07, 2016 |
This post was written by Kristen Willard, M.S.
Debbie Bennett, RRT, BS is the supervisor of Pulmonary Rehabilitation at Barnes Jewish Hospital. A Magnet hospital with more than 1,300 beds, Barnes Jewish in St. Louis, MO is one of the largest hospitals in the United States. With 53,000 inpatient admissions annually, their respiratory therapists (RTs) are in high demand, serving both inpatient and outpatient populations.
As is the case with many with COPD, the patients seen by Bennett and her team are caught in the dyspnea spiral; shortness of breath leads to a decrease in activity, which leads to increased shortness of breath and a further decline in activity. “Many of our patients are so deconditioned,” Bennett says, “that by the time they start PR, they are limited in their activities of daily living.”
There are two ways PR can help these patients with moderate to very severe COPD. First, PR programs help to build endurance and strength through physical reconditioning. The second key component, Bennett says, is helping patients to better self-manage their COPD; in turn, this helps to reduce both index hospitalizations and readmissions. Given the importance of patient education, in 2014, the Barnes-Jewish PR staff set a goal to improve the quality of their COPD patients’ educational experience. They asked themselves two important questions:
1. Are we currently doing the most we can with respect to patient education?
2. How can we better prepare our patients to manage their disease?
A new QI project was born. The team incorporated the principles of Lean Six Sigma, an organizational quality improvement methodology that is designed to achieve outcomes through the systematic review of processes and reduction of variability.
They determined that every COPD outpatient enrolled in their non-transplant PR program would be included in this pilot program.
Here’s what they did:
Revamped their educational approach. During what is known as a rapid improvement event (part of the Lean Six Sigma methodology, which encourages dramatic change in a short time frame), project leaders convened a multidisciplinary team (that included a member of the hospital’s patient experience team) to review the group’s existing approaches and educational materials. The group engaged in role play and process mapping to gain a better appreciation for areas for improvement and considered the evidence base for factors such as delivery of content (e.g., teach-back device training) and sequence of presentation.
This approach produced a standardized library of educational and assessment materials as well as set processes for engaging, educating and empowering patients. A set curriculum was created that could still deliver personalized content to each patient. For example, oxygen use is discussed with each COPD patient; however, if the patient is currently prescribed oxygen therapy, the educational content would be more extensive than for someone who is not. All patients receive information on the COPD PPRN, testing for Alpha-1 and opportunities to become a COPD advocate. The team also developed a welcome script to engage the new PR patient. They created “education stations,” where an RT can spend dedicated one-on-one time with a patient in order to better communicate and discuss content; educational materials and curriculum binders are housed nearby for quick provider and patient reference. Signage alerting staff and other patients to “sessions in progress” were also created to minimize interruptions.
Processes were defined and modified. For example, the group mapped the timing of their current educational sessions and identified that information was only being delivered at two main points in the patient’s PR experience. Given the importance of reinforcement of information, this was less than optimal; the group adapted this approach to deliver education over the course four sessions.
Trained and Supported Staff. Each RT needed to be able to deliver the educational package and learning aids 1) appropriate to the patient and 2) in a consistent manner. Project leads met with staff as a group over three sessions to review materials and processes. They employed role plays as part of the learning process and shadowed clinicians to help them when they needed real-time support in implementing the new approaches.
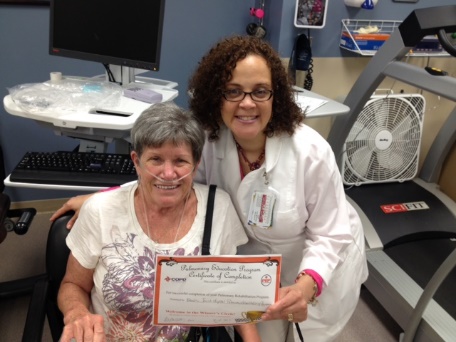
Implemented Quality Measurement. Prior to the initiation of this new program, the PR team was not measuring patient understanding of key disease-related information. To address this gap, the team devised a questionnaire; patients enrolled in the program completed the questionnaire at baseline and then at the conclusion of their PR participation. The Barnes-Jewish team set targets for their work: they aimed for 100 percent of their patients to demonstrate basic disease management skills at program discharged (reflected by a questionnaire score of 90 percent or higher).
Results: The program has realized its intended outcomes. After implementing this new educational approach, the team reported 100 percent achievement in disease management skills in six of the next seven PR cohorts. Staff feedback has also been very positive. They report feeling more confident in their patient education and finding a new appreciation for the intricacies of process improvement. “Much of the success of this process improvement is the result of encouraging each member’s participation and our ability to build consensus around the objectives. Our patients and therapist are all reaping the benefits of our educational enhancement.”
This page was reviewed on March 3, 2020 by the COPD Foundation Content Review and Evaluation Committee