Exercise for Someone with COPD
Always check with your health care professional before starting any exercise program or new activity. The information on this page is not meant to replace a medical evaluation or information from your doctor. You should ALWAYS talk with your doctor about any exercise program before you start it. Your doctor can help you know how much and how often you should exercise.
We all know we should exercise. But it is easy to find excuses for not exercising. We're too tired. We don't feel well. We can't find the time. And many of us just find it too boring!
In addition, if you have COPD you may think that you can't exercise. You may think it will make you feel too short of breath. Or you may feel that it is not safe for you. You may think it will make your lung disease much worse. Actually, avoiding exercise can make you more unfit. You lose fitness when you stop exercising. The less you do, the less you are able to do.
It’s normal to feel this way if you’re short of breath with COPD. However, exercise, done correctly and safely, is one of the best things you can do to be less short of breath. Shortness of breath is called dyspnea (disp-nee-yuh).
Almost all individuals with COPD have dyspnea when they exercise, and because of it, they tend to do less and less. The less they do, the less they are able to do, and eventually the muscles used to perform everyday activities (mainly the muscles in the legs) become too weak to do much at all. This is called progressive de-conditioning. De-conditioning is losing fitness from lack of exercise.
Staying Active at Home/Upper Body Exercises

Remember to consult your health care professional before beginning any new exercise or activity.
Staying Active at Home/Lower Body Exercises

Remember to consult your health care professional before beginning any new exercise or activity.
Remember to consult your health care professional before beginning any new exercise or activity.
An April 2020 recommendation from Harry Rossiter, PhD (UCLA) on the Pulmonary Education and Research Foundation website addresses safe exercising while staying at home during the time of COVID-19.
Exercise itself cannot reverse COPD, but it can change the way you feel, breathe, and function.
At first, your exercise routine should be slow and easy. Even if you think you can do more, take it slow. Your muscles are not used to working like that! Your exercise time and effort should gradually increase over time - each day, do a little more. When you’ve reached the point that you’re feeling better and breathing better, don’t stop. Keep it up at least three days a week.
Exercise cannot reverse lung disease but it can reverse de-conditioning and improve your quality of life.
If your health care professional has told you to use oxygen with activity, you should also use oxygen with exercise. Your usual oxygen flow rate (the number you set on your oxygen machine) may not be enough for you during exercise. Ask your health care provider how to set your oxygen for exercise.
But First, Talk With Your Doctor
Before you start an exercise program you need to talk about it with your doctor. Your doctor may want you to have an exercise tolerance test. This is done using a treadmill or stationary bike. The test helps decide how much exercise you can do safely. Your heart function and how well oxygen is getting to your body will be measured while you exercise. You doctor may then give you an "exercise prescription." This will have details about how hard, how long and how often you should exercise. If you have moderate to severe COPD, your doctor may refer you to a pulmonary rehabilitation program if one is available in your area. Most people with COPD will have better results from an exercise program if it is performed as part of a pulmonary rehabilitation program.
Starting an Exercise Programplus
After you've talked with your doctor and after you've learned better breathing techniques, you are ready to consider an exercise program. Getting started can actually be the hardest part. Let's work through the excuses you may be using to avoid starting an exercise program.
- You may think you are "too tired." Exercise can actually help you feel less tired and give you more energy.
- You may think you are too busy. Think about all the things you do in a day. How much time do you spend on each of these things? How many of these activities are more important than your health? To start, you only need to find 20 minutes in a day (Over time you can increase to 30, 45 or 60 minutes.)
- You may think you are too sick to exercise. Ask your doctor to create a program that is right for you. The right exercises can actually help you feel better and less sick.
To start a program, consider what you like to do. Exercise is easier if it is fun for you. Consider asking a friend or family member to join you.
You may feel short of breath when doing your daily activities. If you do, you will need to begin your exercise program slowly. Your program should be supervised.
If you are fairly active you can create a program that will improve your strength. You can create a program that will improve your ability to be active for longer periods.
Start by making personal goals. Think about these questions:
- Do you want to decrease your feelings of being short of breath during your daily activities?
- Do you want to have energy to join in family, social or professional activities?
- What specific activities do you want to be able to do again?
What is a Good Exercise Program?plus
An exercise program should have:
- Warm up and stretching:
This will prepare you for the exercise. It will also help prevent injury. Doing the right stretches will get your body ready to exercise safely and improve your flexibility. It is good to stretch five times a week. Breathe in before you stretch. Breathe out while you hold the stretch. Hold each stretch for 10 to 30 seconds, if possible. Repeat each stretch three to five times.
- Endurance exercising:
Endurance exercising increases your general physical condition. There are many ways to do this type of exercise. You can ride a bike, walk on a treadmill, pedal with your arms, or use a sit-down stepper or rowing machine. To begin, your exercise routine should be slow and easy. Even if you think you can do more, take it slow. Your muscles are not used to working like this! Your exercise time and intensity (how hard you are working) should gradually increase over time. Each day, do a little more, even if you add just one minute each time. Warm up first. You can do this by going slow and easy for three minutes. You should also cool down at the end of your exercise for three minutes. Ease into it and ease out of it. That is, do not start fast and do not stop suddenly when you are at a faster speed. When you’ve reached the point at which you’re feeling better and breathing better, don’t stop your exercise routine. Keep it up at least three days a week.
- Muscle strengthening:
Stronger muscles will help you be more active with less effort. Muscle strengthening can be done using free weights, resistive bands, or weight equipment. There are muscle strengthening exercises for the upper body and lower body. Strengthening leg muscles will help you stand and sit more easily and help with your balance. Strengthening the arms and shoulders will help you get dressed, take a shower, and do housework more easily. It’s best to do this type of exercise three times a weekm or every other day. Repeat each strength exercise no more than 10 times (10 repetitions). When that becomes easy, add a small amount of weight, just a pound or two. Do not add more repetitions.
To get the most benefit, you should exercise on a regular schedule. You will receive the most benefit from doing a moderate amount of activity on most, if not all, days of the week. But you will still have some benefit if you only exercise three times per week.
Using Oxygen With Exerciseplus
If you are currently using supplemental oxygen, you will need to exercise with it. Your health care provider has prescribed an oxygen “flow rate” for when you are resting and maybe a higher flow rate for activity. Ask your healthcare provider about the best flow rate for you to use with exercise.
Before starting an exercise program, ask your health care provider if you may change your oxygen flow rate during exercise. Ask how high or how low you might adjust it in order to keep yourself at a safe oxygen level.
Set your flow rate as directed about five minutes before you begin exercising. If the exercise is too intense for you, your oxygen flow rate may need to be adjusted, or you may just need to slow down. Do not adjust your oxygen flow rate without talking with your doctor.
How Will I Know if I Am Exercising Enough or Even Too Much?plus
Exercising at a moderate level will help you increase your endurance. This means it will help you be able to be more and more active.
The "Borg Scale of Perceived Exertion with Exercise" can help you decide if you are exercising at a moderate level. "Perceived Exertion" means: how hard you think you are exercising. It can help you stay at a moderate level of activity.
You do not need any special skills or equipment to use the Borg Scale. Using the scale allows you to check on how you are doing without checking your pulse rate.
When you are exercising, try to estimate how hard you think you are working. Don't think about any one factor such as leg pain or shortness of breath. Focus on your inner feeling of effort. Rate your effort as honestly as you can.
Borg Scale of Perceived Exertion
- 0: Nothing at all
- 0.5: Very, very weak
- 1: Very weak
- 2: Weak (light)
- 3: Moderate
- 4: Somewhat strong
- 5: Strong (heavy)
- 6: -
- 7: Very Strong
- 8: -
- 9: -
- 10: Maximal (the most you can work)
Your goal should be to exercise at a 3 or 4 level on the scale.
When Should I Not Exercise?plus
When you are seriously ill, a very low level of activity is best. This may include sitting in a chair and minimal walking. When you have recently been in the hospital, you will need to be supervised during light walking and light weight training. When you are having unusual symptoms, lower your exercise level. Talk with your doctor. The following may be helpful to sort out symptoms that may or may not be consistent with safe exercise.
Yes, Safe to Exercise
- I feel tired
- I feel shaky
- I have a headache
- I am coming down from a steroid burst
- I am too busy
- I am bored and feeling lazy
- I am having a bad day
No, Not Safe to Exercise
- I feel nauseated
- I am having leg pain that I cannot explain
- I am having chest pain
- I am out of oxygen
- I have a fever or strep throat
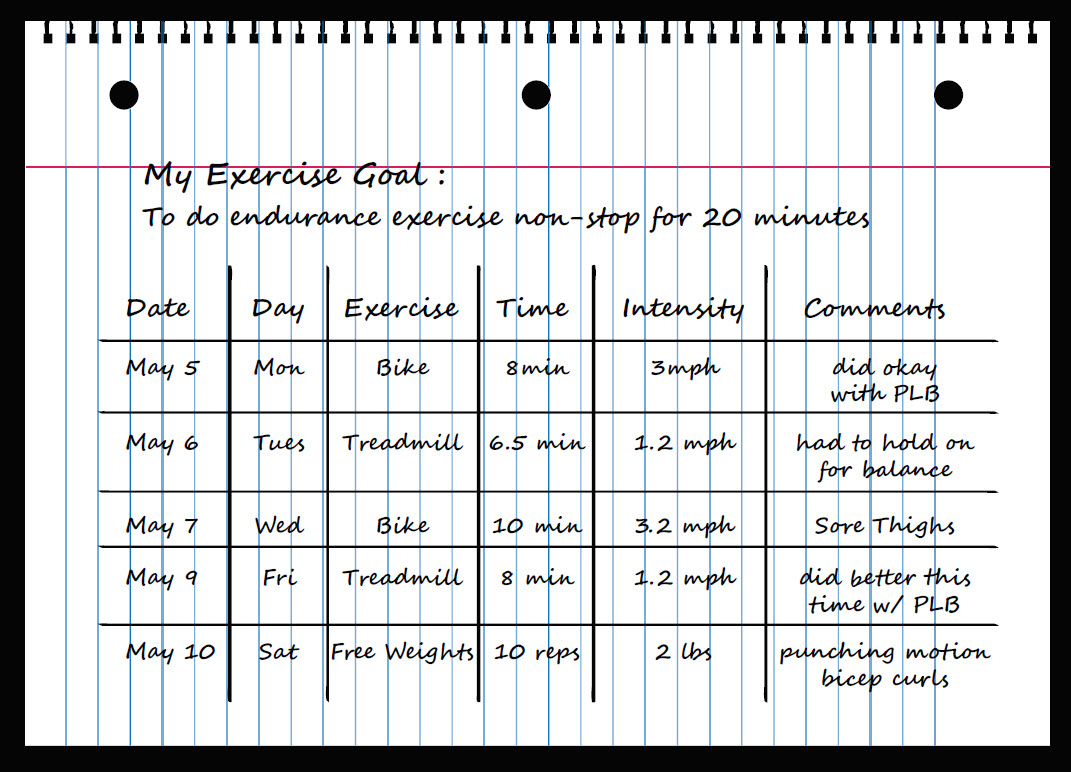
Tracking Your Progress
Many people find it helpful to keep a record of their exercise. You can record when you exercised, how long and how hard. As you improve, these records will encourage you to continue. Reward yourself when you reach small goals.
You may also want to consider if you prefer to exercise alone or in a group. Some hospitals have support groups for people with lung disease. They may allow you to exercise together in a supervised setting. Mall and recreation centers also have walking clubs and group classes. Exercising with others can be motivating.
Finding an exercise program you can stick with can be hard. The key to success is finding something that is fun for you. And don't forget to reward yourself when you reach small goals. Reaching these small goals can be steps to reaching your larger goals.
Here is an example of an exercise goal and a simple exercise log. Ask your health care provider if you should include additional information in this log.
The information on this page is not meant to replace a medical evaluation or information from your doctor. You should ALWAYS talk with your doctor about any exercise program before you start it. Your doctor can help you know how much and how often you should exercise.