Promising Practices in COPD Care: Carolinas HealthCare System
Atrium Health (formerly Carolinas HealthCare System) is one of the leading healthcare organizations in the Southeast U.S. and one of the most comprehensive not-for-profit systems in the country. The health system includes more than 900 care locations and holds more than 40 hospitals. As you might imagine, their care locations are diverse in size and purpose – there are rural and urban locations and everything from academic medical centers to physician practices across the region. Dr. Dan Howard, Pulmonary Disease and Critical Care Medicine and Dr. Amy Clary, Vice President of Partnerships, gave us a peek into the successful COPD care and readmissions reduction program they implemented at Carolinas HealthCare.
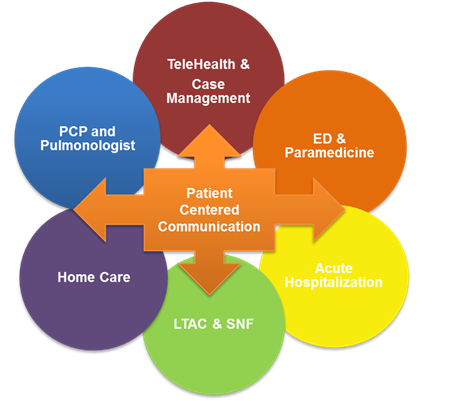
The CHS COPD initiative employs a patient-centered, cross-continuum approach, starting with the provider closest to the bedside and extending beyond discharge. Dr. Dan Howard used the GOLD criteria to build treatment pathways across the care continuum and linked these evidence-based practices with patient centered communication. These pathways are used by all staff engaging with COPD patients. In addition, CHS developed a COPD-specific transition tool to improve communication between providers and venues (see figure).
To develop this patient-centered communication tool, the CHS team pulled together representatives in each care area. This team identified the key patient variables most essential to be communicated from provider to provider during any care transition:
- GOLD Level
- Current medications
- Care management notes
- Patient education received
- Signs/symptoms of exacerbation
- Readmission risk score
- Patient goals (not the provider’s goals, but the patient’s goals; for example, walk to the mailbox)
- Last pulmonary function test results
- Oxygen use
- Discharge disposition
The development of a COPD Data Mart and Scorecard for disease-related, symptom-related and utilization-related outcomes also provides consistent feedback about the impact of the initiatives.
The approach, while still in the pilot phase as of this posting, produced tangible and favorable results. When acute care order sets were used (n=261), the readmission rate was 12.5%, well below the average all-cause readmission rate for patients with COPD of 20% (AHRQ Statistical Brief #196). CHS also registered an 18% decrease in costs to care for these patients. Clary believes this can be attributed to getting the patient on the appropriate medications during the acute care stay, improving their health outcomes post-discharge.
The work is not without challenges. The complexity of the patient population and the many comorbidities with which they present can complicate care. “However,” Dr. Clary adds, “by reducing variability in care for this population, we can better understand how to support patients and families. [Ours is] a system approach that spans beyond any one location, but is a concerted effort.”
Drs. Howard and Clary say patient stories are the most rewarding. When patients share how the CHS team has impacted their life and eased their fears, it is a source of pride for this invested team who has worked hard to improve their patients’ health and quality of life. And that team has earned this; they are all involved from admission to discharge. “The more you involve the entire team across the span of care,” Clary says, “you will discover the best solution for the patient.”
This page was reviewed on March 3, 2020 by the COPD Foundation Content Review and Evaluation Committee