By Danny Pham, PharmD, BCPS, BCACP, BCGP
Inpatient Care Transitions Pharmacist
Baylor Scott & White Medical Center – Plano
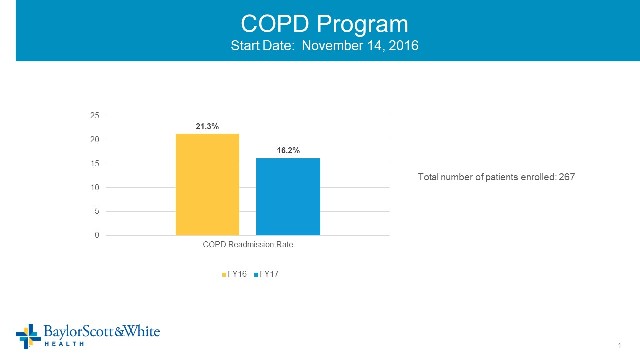
Before we started our COPD program at Baylor Scott & White Medical Center – Plano, our readmission rate was similar to other institutions across the country. We knew there was more we could do to help our patients better understand their condition, be more engaged with controlling their respiratory symptoms, and take a proactive role in slowing the progression of their disease. We also knew that in order for the program to be successful, we had to make sure all members of the team had a good understanding of each other’s roles. Another challenge was how to best incorporate varying levels of expertise to work within an integrated COPD care model.
How does the program work?
In our program, preventing COPD readmissions starts the moment the patient steps into the hospital. After a patient is identified, respiratory therapists reconcile which bronchodilators the patient was on prior to their admission. They also discover any inappropriate use of inhalers and/or poor adherence, provide education using a COPD action plan, and work with the pharmacy team to optimize COPD treatment once patients are stable before their discharge home.
As a pharmacist, my role is first, to determine if patients were on optimal therapy prior to their hospitalization based on the GOLD 2017 updates. I then work closely with our hospitalists to tailor COPD treatment for home, based on the specific needs of the patient, side effects, their preference of inhaler device, and of course, cost considerations. Our team provides education on proper inhaler techniques and teach-back at discharge for inhalers patients were on before they were hospitalized as well as for new ones recently changed or added.
Identifying barriers before discharge
Prescriptions can be sent to our Baylor Scott & White – Plano outpatient pharmacy, where the medication concierge program delivers newly prescribed medications to the patient at bedside before they even leave the hospital. Not only does this serve as a convenience to our patients, it helps us identify issues with cost early on and allows our team to troubleshoot financial barriers which may lead to poor inhaler adherence. Our care management team offers information on resources for financial assistance to help with the affordability of breathing treatments.
The care management team and Jennifer Kyser, BSN, RN-BC, our readmission outcomes manager, work closely to schedule follow-up appointments and pulmonary rehab, set up home O2 for those who qualify, and schedule patients with a new provider if they do not currently have an outpatient pulmonologist or PCP to manage their COPD.
Transitional care services involve a paramedicine team and many others
Jennifer also enrolls eligible patients who decide to opt in for our outpatient transitional care services. The community transitional care team includes Plano Paramedicine and Baylor Scott & White advanced practice practitioners. Josh Clouse, Plano Community Paramedicine Coordinator, and his team worked with us to help develop this Paramedicine COPD program. The program is an extension of our COPD efforts in the hospital with a few important additions. They make house visits to conduct wellness checks, draw labs, collect medication reconciliation, and help identify risk factors for readmissions. The paramedicine team reinforces the patient’s understanding of their condition, promotes self-care to better manage their COPD, assesses proper inhaler techniques, and helps patients avoid environmental triggers that may exacerbate their condition (e.g., checking air filters and reducing dust around the home).
Training for the paramedicine team consisted of time spent shadowing Dr. Omar Awad, one of our Health Texas Provider Network pulmonologists, in his outpatient clinic, learning from respiratory therapists in the pulmonary rehab clinic, and observing our hospitalists provide bedside care for patients with acute exacerbation of COPD (AECOPD). Dr. Mark Millard, medical director at the Baylor Martha Foster Lung Center was also gracious enough to have us shadow his team of highly skilled respiratory therapists for our program. Dr. Millard has been instrumental in mentoring and educating many clinicians to better serve our community for patients with COPD. This partnership between the paramedicine team and our outpatient pulmonary services was pivotal in creating the Paramedicine COPD program. Our emergency department team also provided valuable input regarding treatment and monitoring parameters for patients with acute symptoms who may fall in between the Yellow/Red Zone of our COPD action plan.
A successful readmissions reduction program requires the coordinated efforts of individuals from various disciplines who are passionate and knowledgeable about respiratory care
Addressing pertinent co-morbidities and psychosocial factors in the outpatient setting is crucial to the success of any COPD program. Josh and his team use the PHQ-9 questionnaire to assess if the patient is depressed. If the patient scores high on the survey and has not been treated for depression, the paramedicine team will notify the PCP’s office to determine if treatment is needed. Paramedicine also assesses the volume status of COPD patients with co-morbid congestive heart failure, and have the option of providing intravenous furosemide in the field based on a physician protocol in use with telemedicine.
The Paramedicine COPD program is still evolving. In the future, our hope is to have firefighters and pharmacy students provide smoking cessation education and follow-up in the homes for those who are ready to quit. The team is also exploring the possibility of administering influenza and pneumonia vaccines in the home with help from a local school of pharmacy.
The role of pharmacy students
Pharmacy students play a significant role in our program. They go on ride alongs with the paramedics to see patients in their homes so they can assist with questions about medications. They also reconcile patients’ medications by comparing their discharge medication list to the medications they have recently filled or actually have in their home. With my direct supervision, the pharmacy students also provide basic pharmacologic recommendations. As you can see, there is a lot of overlap with many of the interventions we provide in the hospital. We’ve learned that patients often require additional reinforcement after discharge, due to limited comprehension, low health literacy, or the often overwhelming nature of their hospitalization.
A unique team
Our interdisciplinary team includes pulmonologists, respiratory therapists, cardiopulmonary trained RNs, readmissions program outcomes manager, LMSW (licensed master social worker) or RN care manager, director of healthcare improvement, CP-C (community paramedicine coordinator), hospitalists, ED physicians, advanced practice providers, physical/occupational therapists and a clinical pharmacist. The team works closely with hospitalists to optimize COPD care for patients in addition to other penalty diagnoses identified by CMS.
The importance of proper inhaler use – a big issue - reinforced by the entire team
In working with this program, the thing that surprised me most is how important it is to reinforce proper inhaler technique prior to a patient being discharged. Some patients we see at discharge have not been properly trained or asked to provide teach-back to demonstrate a thorough understanding of the appropriate use of their inhalers.
It should be the responsibility of prescribers, respiratory therapists, pharmacists, and/or community care team members to assess the patient’s understanding of their condition and ensure they are comfortable with properly using their inhalers. “
"This education was much needed. My inhalers were going to make me bankrupt. Switching me over to a 3-in-1 inhaler was a God send! I’m breathing better now. Thank you very much!”
One patient was using her LABA/ICS as directed, but she thought her LAMA was to be used as needed for shortness of breath. We’ve also had patients who are adamant that their maintenance inhalers do not work. Often this is because they are either rationing them due to cost, or have not been educated on how their long-acting inhalers are meant to be used daily to prevent flare-ups and slow disease progression. They don’t always understand that their rescue inhalers are to be used as needed to treat acute respiratory symptoms, but they also have to know that overuse or exclusively relying on their rescue inhalers to treat their COPD may increase their risk of side effects such as increased heart rate, nervousness, or in some cases trigger irregular heart rhythms. These major knowledge gaps can be prevented at many different levels of their COPD care.
Delivering a consistent message throughout the process
It’s essential to thoroughly train key members of the team to ensure consistency in the COPD education and message being delivered to the patient. For example, it’s unreasonable to expect every pharmacist to know which inhalers contain a LABA/LAMA vs. LABA/ICS or to expect a respiratory therapist to properly educate on every DPI or MDI device available without the appropriate training. The ED staff can be trained to inform patients being admitted for an acute COPD exacerbation that they’ll be started on nebulizer treatments, steroids, and possibly an antibiotic to help reduce their respiratory symptoms. They can also tell them that once they are stable they will likely be transitioned to a maintenance inhaler to prevent further flare-ups and hospitalizations. This will make our jobs easier on the back end when, prior to discharge, we’re trying to optimize our patients’ breathing treatments and educate them on the importance of the daily use of their long-acting maintenance inhalers. Delivering the same message throughout their stay will promote improved COPD self-care and better control of their breathing.
It truly takes a village to implement this program. Our innovative readmissions team focuses on making a difference in the lives of those we care for and we are fortunate to have overwhelming support from our executive leadership team who believe in creating a unique patient experience here at Baylor Scott & White – Plano. We’ve learned a lot and established a great program but we’ll always have more work to do. The program is evolving every day.
This page was reviewed on February 13, 2020 by the COPD Foundation Content Review and Evaluation Committee