This post was written by Jane Martin, BA, LRT, CRT, Assistant Director of Education at the COPD Foundation.
At an annual conference of the American Association for Cardiovascular and Pulmonary Rehabilitation (AACVPR) in Charleston, South Carolina, the COPD Foundation's Jane Martin met Robyn West, a representative of the Breathe At Ease program. She was impressed not only with the Breathe At Ease program outcomes but with Robyn's enthusiasm. Over the following weeks Robyn and her colleagues talked with members of our COPDF Care Delivery Team about this exciting new COPD management program. Here is a summary of that conversation.
What is Breathe At Ease?
Breathe At Ease is Network Health’s proactive outpatient condition management program designed to help members and participants avoid flare-ups, control symptoms and potentially improve their lung conditions. It’s intended to supplement a physician’s care of chronic bronchitis, emphysema and chronic obstructive pulmonary disease (COPD). We partner with respiratory therapists who are experts in the area and work on a personalized individual level with our members.
What is Network Health?
Network Health is a payer serving 22 counties in the state of Wisconsin. Breathe At Ease is available to local Network Health members with a qualifying diagnosis of COPD: chronic bronchitis or emphysema.
Robyn, do you work for the payer?
The registered respiratory therapists are employed through the hospital. Network Health contracts the facilities to better manage their members with COPD.
Where, exactly, is Breathe At Ease currently operating?
We have multiple locations within the Ascension Wisconsin health system and also Holy Family Memorial participating in the outreach to members with chronic lung conditions.
Can you walk us through how this program works for the patient?
- A patient can enroll by contacting one of the Breathe At Ease respiratory therapists to schedule an appointment or ask their doctor for a referral to Breathe At Ease.
- The first thing that happens when a patient enters the program is that they meet with a Breathe At Ease Respiratory therapist for a face-to-face assessment, education and goal identification session lasting up to 90 minutes.
- This is followed with monthly phone calls by a respiratory therapist to follow up on their needs, compliance with their action plan and one-on-one support to help manage their condition. The respiratory therapist answers any questions they have and provides helpful tips to help patients care for their lungs.
What educational tools or approaches do you use?
Goals are established and an action plan is given. The education that is given is personalized and goals are established at each initial visit. Teachback is used along with coaching.
Is all the education done up front or are topics covered on each call?
Education is done at the initial assessment; however, different topics are reviewed monthly. This could include inhaler instruction, exercise regimen, triggers, reminder of vaccines, discussion of a recent doctor’s office appointment, etc. This is a personalized program. The respiratory therapist modifies each program to the needs of the individual.
Does the same RT follow them throughout their time in the program?
Yes.
Do any of the Breathe At East participants use pulmonary rehab?
Many of our members are past participants of pulmonary rehab. Some members simply cannot afford pulmonary rehab and if eligible will opt for Breathe At Ease. Other members start with Breathe At Ease but enroll into pulmonary rehab due to severe deconditioning. At that point Breathe At Ease is on hold. Each individual has specific needs or reasons for enrollment.
How long are Breathe At Ease participants in the program?
A member can be enrolled into Breathe At Ease for two years. After one year they can opt to renew the program for one more year. If at any time the member wishes to dis-enroll, has a change of insurance, change in health status to hospice, the program will be discontinued.
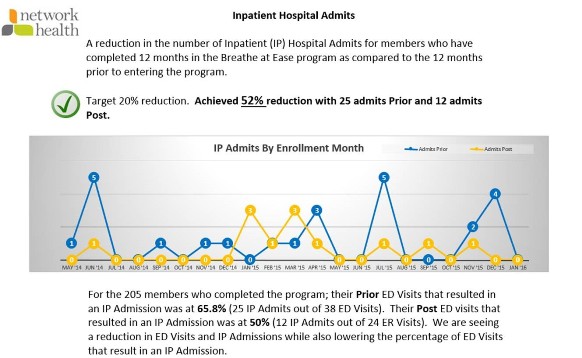
This sounds like a great program, but what about outcomes?
We have a lot of successful outcomes. Here is a summary.
What has been the most surprising result of your program?
The outcomes are not surprising as the more we understand our health, the better our quality of life is. The number of members seeking help and wanting the proper knowledge in regard to COPD management was surprising. It is also surprising how many people do not understand how to properly take their medications or the purpose of each prescription.
What do you see as the most unique aspect of your program?
One is our strong partnership between the provider groups and insurance company. Also, our program takes an individualized approach with each member to educate and empower them to manage their chronic lung condition.
What do you see as the activity and/or aspect of your program that is making the biggest difference?
Building the trust with members along with empowering them to make decisions related to their health makes the difference. The program not only educates members on how to manage their COPD but we serve as their coach, too. A member always knows that they can call with questions/concerns, and they appreciate this service. There is a trusting relationship with each and every one of them.
How many FTEs does your program employ and what are their credentials/experience?
There is a full-time registered respiratory therapist that is a 1.0 FTE. A respiratory therapist travels between five locations to provide the services for our COPD population in outlying locations.
Can you share a brief story about a patient in your program, a success story?
A 66-year-old bus driver with emphysema: the member entered the program with a history of four plus exacerbations, lost work time and was deconditioned. Her main goal was to breathe better. She was taught everything she needed to know in order to self-manage, including controlled breathing techniques (CBTs) with exertion, action plan, how to start exercise and how to keep independence with confidence.
After one year, she had zero exacerbations. She joined Silver Sneakers (an exercise program) with slow progression exercise. She uses CBTs with exertion and has not missed a day of work due to breathing difficulties.
Today, she continues to drive the bus and uses CBTs faithfully with exercise. She continues to try new exercises, including strength and cardio at the YMCA. She is very happy with Breathe At Ease and her confidence in her ability to self-manage her lung condition has increased.
This page was reviewed on March 3, 2020 by the COPD Foundation Content Review and Evaluation Committee