The pharmaceutical companies and the FDA also provided information on the severe side effects that volunteers experienced. In general, those are side effects that are so bad that they stop people from performing normal activities. Most of the severe side effects occurred after participants got the second dose, and these side effects were more common among younger participants.
Among people aged 18 to 55, 4.6% reported severe fatigue after getting their second injection, and 3.2% had severe headaches. Fevers were also common in th8at age group; about 15.8% of the volunteers had a temperature of at least 100.4 degrees Fahrenheit after their second shot. Among volunteers older than 55, 2.8% reported severe fatigue, 0.5% experienced severe headaches after the second dose, and 10.9% had a fever.
We should have more details soon about the COVID-19 vaccine and people with underlying conditions like COPD. Most of the people who are getting vaccinated right now are health care professionals and other front-line workers. The CDC is creating a plan that will give us an idea of when elderly or people with chronic conditions might be able to receive the vaccine.
A new review of all the evidence about wearing masks and possible exemptions for people who might not need to wear a mask has been published in the European Respiratory Journal and confirms the earlier comments made by the COPD Foundation.
The study reported in the European Respiratory Journal found that it was very rare for the pulse oxygen levels of people with COPD to fall when they were wearing a mask—even while walking.
Some states and countries allow people with certain disabilities to be exempt from wearing face masks that are used to prevent the spread of COVID-19--rules that say some people don’t have to wear face masks. You can even buy these “exemption” cards and holders on many web sites for less than $10.
But for people with chronic lung disease this must be carefully considered. Here is what experts in chronic lung disease have to say — "…situations such as chronic pulmonary (lung) illnesses without an active exacerbation (flare), are less clear (as a reason for a mask exemption). An individual with a chronic pulmonary illness is at higher risk for severe disease from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19. Conversely, if that same individual were infected with SARS-CoV-2, he or she would likely also be at higher risk for spreading viral illness because many pulmonary illnesses are associated with a chronic cough. There is a risk-benefit ratio that must be carefully considered."
Before you go online to buy a mask exemption card, talk with your doctor or other health care professional. As noted above, a very few people may not be able to wear a mask--their pulse oximeter readings drop more than a couple points for example. But it is good to discuss this with your health care professional. If you cannot wear a mask, you may have to very carefully choose what you think are safe activities outside your home. Please note that there are scammers that will be happy to take your money for a card without providing you any useful or safe support.
Again, newer information shows that taking your usual COPD medicines that may include inhaled corticosteroids does not increase your risk of getting COVID -19 or make your symptoms worse if you do get COVID-19. It does not seem to prevent COVID-19 either. But it is important for your treatment of your COPD, which you do not want to get worse because you stopped any of your medicines.
Oral steroids are still very important for treating exacerbations or flares and should be used when needed. If you are continuing to have exacerbations or flares you should ask your doctor or clinician if there are any things you can do to help cut down on those exacerbations.
There are several vaccines that are being tested right now. Some are in the third and final stages of studies and may have some results soon. Many of the vaccines require two doses over a few weeks to a month. One that had recent information published is in stage or phase II testing and only requires one dose. The vaccines are being tested to see if they result in the recipient (person getting the vaccine) making antibodies to block the COVID-10 or SARS-Co-V2 virus from infecting the person. These studies are different than the much longer studies that look at rates of infection. Those studies can take many years to complete. The studies of the COVID-19 vaccines will be done in different age groups---usually 18 to 55 years of age and older than 55. Studies or trials in children have not started in the U.S.
The rules about what is okay to do or what businesses and schools can open is still different by state and sometimes by city. Right now the number of new cases of COVID-19 is not yet falling so for people at high risk like older adults with COPD, it is best to continue to limit where you go, avoiding places that are indoors with large groups or even outdoors with large gatherings. Of course, when you do go out to the grocery store or your doctor’s office, wear a mask, and wash your hands regularly.
The CDC’s first recommendation for the upcoming holidays is to keep gatherings small or virtual. Thanksgiving dinner may not be the same but we are all trying to think how to be creative in ways to meet with family or friends for holiday.
There were some delays in getting flu vaccines, especially the high dose quadrivalent vaccine used for older adults, to some doctor’s offices and pharmacies. That seems to have been fixed. You should now be able to get your flu shot and please plan to do so by end of October. Remember, you may want to call ahead to schedule a time to get the shot at your doctor’s office or find a time that the pharmacy is less crowded. Remember you can get the flu shot, any of the pneumonia shots, or the first or second shingles shots that you may need, on the same day.
Two new influenza vaccines have been licensed for use in people aged 65 years and older: a quadrivalent high-dose influenza vaccine and a quadrivalent adjuvanted influenza vaccine. Previously, high-dose and adjuvanted influenza vaccines were only available in trivalent formulations. This will allow older adults to have additional protection against another strain of influenza that may be important this year.
The COPD Foundation, in partnership with the American College of Chest Physicians, American Lung Association, and American Thoracic Society released the following statement in response to the Centers for Disease Control and Prevention (CDC) recommendation for facial coverings to be worn in public settings during the coronavirus disease (COVID-19) pandemic. For more information review the facial covering statement.
Updates from June 9, 2020plus
When the COVID-19 pandemic started, most non-urgent healthcare services were postponed or switched to telehealth when possible. This was done to minimize exposure to the virus and to free up healthcare capacity and personal protective equipment supplies to prepare for a COVID-19 surge. As Dr. Byron Thomashow stressed on our May 21st webinar, COVID-19 does not mean other medical problems no longer exist and importantly, calling it elective medical care does not mean there is not an underlying problem that needs to be addressed.
As the country begins to reopen, healthcare systems have followed suit, expanding the types of care they are offering in-person and restarting testing and surgical programs to some degree. As is the case with your decisions about going out in public, the considerations for whether you, as someone living with COPD, should resume non-urgent medical care are slightly different. There is no universal answer to questions about going to an in-person doctor’s visit, doing your annual pulmonary function testing, resuming evaluations for surgical procedures, and other important care.
Your answer will likely depend on a number of different factors, including if telehealth is still an option for the care you need, how severe the COVID-19 outbreak is in your community, the types of precautions the medical facility has put into place, the risks of waiting if you choose not to seek care, the preparation and recovery process associated with the care, and more. Since no organization can make this decision for you, we have outlined a few critical questions to use as you engage in your discussions with your family and healthcare team. You can access the handout, Considerations for Resuming In Person Healthcare here and we welcome your input on other resources that you would find helpful as we begin to reopen in a time when the virus is certainly still present and circulating in many communities.
Finally, please remember that the best way to prevent COVID-19 is to stay home whenever possible, wear a mask when you go out and always wash your hands frequently!
Updates from May 1, 2020plus
Yesterday we explored what we have learned about COVID-19 symptoms, risk factors and efforts to develop treatments and vaccines. Read on for updates on the efforts to reopen states, why people with COPD might have to wait longer and policy issues that we are following.
Reopening
Most public health experts suggest that it is much too early to reopen most of our country and have suggested several guidelines to use when making decisions about reopening. Efforts to “flatten the curve” have started to work and most public health experts feel that we have reached a plateau, meaning how fast cases are growing and daily increases in the number of deaths and hospitalizations have begun to level off. This does not mean we are out of the woods. Cases are still rising, and the virus is still spreading at a community level in most of the country. If we start to see areas where the percentage of tests that come back positive is declining and hospitalizations are declining, we will be more confident that the situation is improving.
There are some states that have already started to remove some restrictions on businesses and other activities. HOWEVER, it is likely that even when parts of the country begin to reopen, it will be necessary for people with COPD to continue preventive measures for quite some time. People in high-risk populations need to take extra precautions to avoid being exposed to COVID-19 and what level of risk political leaders feel is acceptable for reopening, is most likely not going to be acceptable for these populations. We will continue to monitor the situation and update recommendations as needed, but for the time being, we recommend that people with COPD continue to stay home whenever possible and practice strict preventive practices if they must go out, such as staying at least 6 feet away from others, wearing a face covering and gloves and washing hands often among others.
Policy Issues
All of us in the patient advocacy community are working hard to represent your needs with policymakers at all levels of government who can act to make changes that will help ensure our high-risk communities can stay safe at home and still access the care you need to manage your health in an affordable way. Many changes have taken place already. The Centers for Medicare and Medicaid Services (CMS) has vastly expanded the ability to receive care in your home, including paying for telehealth via phone or video, and by allowing you to receive infused and injectable medication in your home rather than having to go to a clinic. For those who use oxygen, they have also waived requirements for you to be seen in person when you start oxygen and again at the 12-month period. The recent CARES Act included a provision requiring insurers to cover a one-time 90-day supply to minimize trips out and included many financial relief policies that might be useful to you.
The speed with which these changes have taken place has been welcome news, but our job is not over. There are still urgent priorities that must be addressed to help keep you safe and deal with the long-term implications of this pandemic.
One of the most pressing concerns relevant to the COPD community is an effort to ensure people who have COPD and other high-risk conditions who work in jobs that are considered essential, such as healthcare workers, grocery stores and pharmacies, can qualify for paid leave policies in place during the COVID-19 pandemic. Unfortunately, as of now, there are no policies that would allow vulnerable populations to voluntarily take paid leave due to the danger they face by remaining in the workforce, and those that choose to protect their health and quit their jobs would not qualify for unemployment. As more states begin to reopen, protecting our population is even more important. The patient advocacy community recently sent a joint letter to congressional leaders and we will continue to push for this to be addressed.
We are also advocating to ensure you are protected from surprise medical billing and high out of pocket costs should drug shortages arise and you require a medication that isn’t traditionally on your plan’s formulary, or if you seek care for COVID-19 related concerns. Finally, we are joining the calls to urge CMS to cover virtual pulmonary rehabilitation and to empower respiratory therapists to provide services via telehealth. These are issues that would benefit the COPD community even in the absence of COVID-19, but they are made even more urgent in the current situation.
We know there are many more challenges you are facing that could be addressed by policy solutions at the state and federal level. We will continue to monitor and advocate on these issues in the coming weeks and months. Please check-in with the COPD Action Center if you are interested in getting involved or and share your thoughts on COPD360social.
Updates from April 30, 2020plus
It is the end of April and by now most of you have been staying close to home for at least 6 or 7 weeks. The COPD Foundation team continues to follow new information and guidance about COVID-19 and its impact on people with COPD. Last week we held an update webinar with medical experts to review what we have learned about the coronavirus, how COVID-19 is affecting people with COPD, tips for adapting to telehealth visits, and policy changes that might impact how you get care. If you missed the webinar, or just want to review what you heard, you can view the recording and download the slides here.
We know that by now, everyone would like to see significant progress in slowing the spread of the disease and in the development of treatments and vaccines. While progress hasn’t been rapid, we have seen some reasons to hope. Read on for a few updates, reach out with what is on your mind about COVID-19, and keep supporting each other!
Symptoms
There are now over 1 million confirmed COVID-19 cases in the U.S., so we are learning more about its range of symptoms. Recently, the CDC updated its list of official symptoms, adding 6 new possible symptoms to fever, cough and shortness of breath; chills, repeated shaking with chills, muscle pain, headache, sore throat, and new loss of taste or smell. While not listed by the CDC, GI symptoms including nausea and diarrhea have been seen as well.
Risk Factors
Scientists have started looking at large groups of patients in different states or hospitals to study who is most at risk for the disease and serious complications. From these early reports we are learning that women make up a greater proportion of cases, but men are a larger portion of overall deaths. Studies have reported an increased risk for severe complications in areas with higher levels of air pollution, in smokers, and those with underlying health conditions like obesity, diabetes, heart disease, and other chronic conditions.
Early data on COPD shows no indication that people with COPD are at increased risk of catching COVID-19, BUT those that do get the disease face a 5 times greater risk of developing severe complications. Therefore, we have stressed the importance of taking strong measures to prevent all possible exposures to the virus.
Treatment and Vaccine Development
The scientific community is rallying around the urgent need to find new treatments and vaccines for COVID-19. There have been unprecedented collaborations among academic scientists, industry, and government agencies. Data on COVID-19 related studies is being disseminated rapidly thanks to relaxed publishing policies at many journals. There are indeed reasons to hope, however, caution is still warranted because scientific discovery takes time, SARS-CoV-2 is novel, and it is imperative that any treatment or vaccine is studied rigorously to avoid causing harm to the public.
Repurposed treatments are those that have been or are currently being used for other conditions, but scientists have a reason to believe they could be helpful in COVID-19. This category includes the often talked about chloroquine, hydroxychloroquine and others. Initial optimism by some has given way to warnings of limited effectiveness and the potential for harm based on a recent study of veterans who were given hydroxychloroquine. Limited data on the benefits and harms of these treatments in COVID-19 is just one reason why NO treatment should be tried unless you are under the care and direction of a healthcare professional.
There are also many new investigational drugs and supportive therapies being studied, including some that were already in advanced trials for other viruses such as Remdesivir, a drug being studied as a potential Ebola treatment that seems to shorten the number of symptomatic days in early data released by the NIH. They are also studying treatments for specific complications of COVID-19 like acute respiratory distress syndrome and the cytokine storm. Many companies are beginning preclinical (before human trials) work on antibody treatments that would use the blood or plasma of COVID-19 survivors.
On the vaccine front, efforts are underway in several countries to identify candidates that can be studied in human trials. Most are still in the preclinical stage, though some have recently completed animal testing and are set to enter phase 1 clinical trials in humans (studies done on healthy volunteers to determine safety). Just this week, a team from Oxford University reported promising results of a vaccine candidate that was effective in monkeys and will soon be moving into human trials. A collaboration in Germany began human trials on April 23rd, 2020 and hopes to begin trials in the U.S. soon. While there is still a small chance that these advanced efforts could result in a vaccine in late 2020, it is important to recognize that it will likely still be well into 2021 before a vaccine is widely available. If a vaccine was indeed proven to be safe and effective and then manufactured and distributed in 2021 it will mark one of the fastest timelines ever seen. Some efforts are already underway to prepare manufacturing capacity in hopes that vaccines being studied will prove to be effective.
If you are interested in doing a deep dive into treatments and vaccine development, there are several comprehensive resources to check out. The Mayo Clinic has a good explanation of how a vaccine is developed and the different types of vaccines being looked at in COVID-19. The Milken Institute has a COVID-19 tracker and STAT News has a thorough review of all the different treatments being studied.
In part two we will explore updates related to reopening the country and policy issues that could affect people with COPD.
Updates from April 8, 2020plus
Crisis Planning and Healthcare Decisions
During the COVID-19 crisis, our healthcare systems are being asked to operate in a way that they have never had to before. Visitors aren’t allowed to be with patients, doctors trained in one specialty are being redeployed to COVID-19 care, and hospital administrators are scrambling to find ways to handle spikes in patient volume and the need for ventilators. Our hospitals and the healthcare workers are navigating uncharted waters along with the public.
In times of crisis, it is impossible to deny the increase in anxiety and fear, even among the most optimistic and even when we see stories of generosity and reasons for hope on the horizon. One of the issues generating anxiety among people with disabilities and chronic diseases is the fear of the healthcare system being overrun, causing some to be denied life-sustaining care. Avoiding these situations is the driving force behind “flattening the curve” so that the peak demand for hospital beds and ventilators is lowered and the number of people with the disease becomes more manageable.
Across the country and throughout the world, people are doing everything within their power to prevent disease transmission and treat those who get the disease. It is also important to keep in mind that only a small portion of those who do catch it, will end up requiring hospital admission or a ventilator. Despite these efforts, there are areas of the country where disease activity has begun to strain the healthcare system. You have likely seen media coverage on how states and hospitals are starting to make plans to handle difficult decisions around ventilator or ICU bed shortages.
We think it is important to address this sensitive subject up front so that the healthcare professionals can make the best possible decisions in a time of crisis and so that your families and you are empowered with the information you need to advocate for your needs in the very unlikely event you are faced with these circumstances.
Here a few things to know about HOW decisions about who receives medical care would be made.
- Some states have released guidelines and others have not, but hospitals are making their own plans to clarify how they will implement guidelines. Many hospitals will consult with their ethics committees to make these plans.
- These are CRISIS plans, meaning they should only go into effect when NO other alternatives can be found. They are not plans meant to preserve ventilators just in case they might need them for someone else. They are applicable when there is a severe shortage of ventilators, physicians and ICU beds, and are designed to help people make decisions so that the greatest number of lives can be saved. To keep from needing to activate their crisis plans, cities and states are actively seeking new resources and hospital capacity outside of their walls. The exception to this might be if multiple physicians agree that there is no chance of survival and death is imminent with or without a ventilator. In that case they may decline to intubate someone, not only because it would be an inappropriate use of a scarce resources, but equally important, to prevent needless suffering for a patient with no chance of survival.
- Decisions will be made in teams and multiple physicians will have to agree on making decisions to withhold treatment that will not help the patient.
- Your status as a COPD patient in itself, should NOT be factored into the decision-making process. That means that no physician could say, that because this patient has COPD, they are going to the bottom of the list for an ICU bed or ventilator. This applies to patients with heart, liver, or kidney disease as well. Each patient must be evaluated on their own merits. COPD by itself is not an exclusionary criterion to withhold a ventilator. The severity of COPD in the context of the patient’s entire medical history is what is important. Chronic disease communities are fighting to ensure that inappropriate withholding of treatment of patients with various medical conditions should not happen, and recently the Office for Civil Rights at the Department of Health and Human Services issued an opinion that reinforced the fact that states must make these decisions medically and legally appropriately.
- Decisions will be made based on certain objective criteria of a person’s condition and organ function, combined with an element of clinical judgment if a patient can reasonably be expected to survive. It is entirely possible that a patient with COPD and COVID-19 infection might be placed on a ventilator because of a better chance of survival than a patient with previously normal lung function but who is sicker because of COVID-19. That is why these decisions must be individual and objective based on current health status.
In these circumstances it is important for everyone, not only patients with COPD or other chronic illnesses, to prepare an advanced care directive with guidance of their physicians, and to engage in comprehensive conversations about treatment goals. This is particularly important for patients who are ill. We offer more details on preparing advanced directives (living wills and durable medical power of attorney) in this guide. Most hospitals are bringing in more palliative care specialists to talk with patients and families (virtually) to have you identify what matters to you most and how you would want specific medical scenarios to be handled. These conversations are difficult but critical, and not just in a time of COVID-19.
99% of the time you or your loved one will not face a circumstance that requires this knowledge, but preparation will enable the best possible outcomes. So, what should you know and ask in the unlikely case that you or a loved one fall seriously ill with COVID-19 in a stressed healthcare environment?
- Due to COVID-19, most hospitals are not allowing any visitors, even close family. It is important to bring your cell phone and a charger to the hospital if you must go and to establish contact between your care team and your family via phone or video chat if possible. Doctors are doing their best to keep the communication flowing but do recognize they might be in crisis mode and overwhelmed.
- Ask your care team or have a family member ask for the hospital to share their written policies and how they are handling the potential for healthcare resource shortages.
- If you find yourself or a loved one in a situation where no ventilator or ICU bed is available, look and ask for options to make sure all possibilities have been exhausted. Don’t hesitate to ask questions. Have they checked nearby hospitals, could the patient be transferred if options exist nearby? Are there any available ventilators that might be brought to you if transferring to another hospital isn’t possible? Were experts in COPD (or another underlying chronic condition) consulted about the patient’s treatment plan? Will the decision be changed if new resources become available?
It is understandable to be concerned about COVID-19. We know you are running through many questions about what would happen to you or your families if you get the disease and we encourage you to leverage the content we have created on our Coronavirus Information page. Preventing the disease is the most effective way to avoid negative outcomes, but it’s important to realize that if you do end up getting COVID-19, hope is not lost. Arm yourself with information, follow the advice of medical professionals and know that the overwhelming likelihood is that you will have access to all of the best care and treatment that is available to help you fight this disease.
Updates from April 3, 2020plus
Today we updated the answer to question 61 in our FAQ document (hyperlink to document). Please remember that recommendations change as new information becomes available. We will continue to evaluate new information and update the FAQs regularly.
Should I wear a face mask? Does it matter what type of mask?
A. You should cover your face when you are around other people outside your home (examples: an elevator, a store, a crowded street). It is important to understand that the primary purpose of covering your face when you go out of your home is to prevent your own respiratory droplets from infecting others. Currently, the CDC recommends that only people who are sick or are caring for sick patients need to wear masks. However, on April 3rd, the CDC issued a new recommendation that people consider wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies) especially in areas of significant community-based transmission.
Since COVID-19 might be contagious in the days before someone experiences symptoms, more public health and medical professionals are recommending that people cover their faces when in public. Unfortunately, there is not enough evidence to definitely say if wearing a mask will protect someone from contracting COVID-19, so public health professionals are relying on the best available information and adjusting their suggestions as new information emerges.
It is important to note that while you should consider covering your face, we are NOT recommending the use of medical masks such as surgical masks and N95 masks. These are critical supplies that should be reserved for the healthcare and first responder workforce who face a much higher risk of catching COVID-19 due to their close physical contact with infected patients. Additionally, medical masks are often used incorrectly or not properly fitted to the user, making them less effective for the general public. Covering your face while you are out of the house is NOT a substitute for other precautions. Cloth masks do not filter out the virus. You still need to regularly wash your hands, stay home whenever possible and stay at least 6 feet away from others.
Many people with COPD or other lung diseases have a hard time breathing with masks on, especially the N95 masks. If you use oxygen, it may be even more difficult to wear a mask properly. If you can tolerate it, there does not appear to be other downsides to wearing a face covering of some type (washable scarf or home-made face mask), and it may help remind you not to touch your face while you are out as an added benefit. So, wash your hands often before and after you cover your face and check out these ideas to find a face covering that will be comfortable enough to wear if trips outside of your home are essential.
- Consider using a cloth mask. Many organizations are organizing groups of volunteers who are sewing cloth masks. If you sew, you can find instructions on sites like this one (https://www.nytimes.com/article/how-to-make-face-mask-coronavirus.html or consider asking for a donated mask via your neighborhood email list-serv, community-based organization or other local resources. It is recommended that cloth masks be made from 100% cotton, percale or denim and consist of at least 2 fabric layers.
- If you cannot use a cloth mask comfortably, try a standard bandana with hair ties to hold it on. There are tutorials online such as this one https://youtu.be/EAj12GKuAEk.
- When in doubt, reach out to your healthcare team to ask for suggestions based on your individualized needs.
Updates from April 2, 2020plus
This week, the Centers for Medicare and Medicaid Services (CMS) made several important changes that people on supplemental oxygen or those who receive a new prescription during the COVID-19 emergency should be aware of. These changes were requested by the patient, healthcare professional and supplier communities to reduce potential COVID-19 exposures faced by those on oxygen and other medical equipment in the home.
- You will not be required to sign for your oxygen delivery. Most companies have moved to contactless delivery wherever possible. If your supplier asks you to sign something, politely remind them of the new rules and maintain a minimum of 6 feet between you and the delivery personnel.
- CMS waived the requirements for in-person evaluations for new oxygen prescriptions as well as the “recertification” visit that is typically required 12 months after your initial prescription or when equipment is swapped out due to reaching the end of its useful lifetime, or about every 5 years. You may be requested to complete these visits via telehealth or after the COVID-19 health emergency has ended.
There were several other changes made to how payment rates are calculated and some enhanced flexibility for suppliers that are designed to make it easier for them to respond to enhanced demand for short-term oxygen needs related to COVID-19. We are aware of media articles that suggest some areas of the country could face a shortage of oxygen, however, at this time there is no evidence of any supply issues for home oxygen compressed cylinders. We are monitoring the situation and will communicate any future challenges with you as needed.
We also ask that if you are experiencing trouble accessing the oxygen you have been prescribed, consider sharing your story with us. You can email statecaptains@copdfoundation.org or share it with others on COPD360social.
Updates from April 1, 2020plus
COVID-19, social distancing, and your medical appointments
During the COVID-19 pandemic, the most important action you can take is to minimize the chances you can get the disease in the first place. Perhaps equally as important though, is maintaining your health, including managing your chronic diseases like COPD.
If you had routine medical appointments scheduled or if you find yourself needing to check-in with your healthcare team for new concerns, telehealth or virtual visits may be an option. Policymakers, insurance companies, and healthcare professionals have been working hard to make it easier for you to access care virtually. In the past, there were many rules about how telehealth services could be provided, what services could be offered and who could offer them. These rules limited telehealth availability because in most cases, healthcare professionals wouldn’t be paid for the services they were providing outside of these rules, and this was especially true for telehealth services provided to people on Medicare.
In the days since the COVID-19 outbreak started, big changes have been made, mostly on a temporary basis. Here are just a few highlights that should make it easier for you to access care without leaving your home. These are applicable to people on Medicare BUT most private insurance plans have committed to following Medicare’s lead and making telehealth more widely available if they haven’t already.
- You can now receive telehealth services in your home. Previously, many billable telehealth services had to be provided in an office setting as it was mainly intended as a way for people in rural areas to access specialty care in conjunction with their rural care.
- You can now access telehealth services on a mobile phone, tablet or video-enabled computer. While two-way video communication is the ideal method, phone-based consultations are now considered acceptable and your doctor can bill for the visit.
- New patients now qualify for telehealth services. Previously only people in an established relationship with a provider could qualify.
- If you have a high-deductible health plan, your plan is allowed to waive costs for telehealth services even if you haven’t met your deductible, so check with your plan to see if they are offering this benefit.
- If you usually have to travel to a specialist outside of your state, you can now receive care from them via telehealth. Previously providers could not offer telehealth services to out of state residents.
- Congress set aside funding for rural networks, community health centers, and others to increase their capacity to provide telehealth services so hopefully access in these areas will improve soon.
If you have a routine appointment scheduled, reach out proactively and see if it can be held via a virtual visit or teleheatlh. If that is not possible, we recommend you consider postponing any appointments that are not medically required in the short-term but make sure to discuss the implications of rescheduling with your healthcare team to weigh the risks and benefits.
Have you received care via telehealth? Consider sharing your experiences and tips for making the most of your virtual visit on COPD360social so others can prepare.
Updates from March 29, 2020plus
As more information becomes available about COVID-19, updates will be made to our question and answer document. Today we updated the answer to question 22 and have copied it here as well. Please visit the Q & A document (pdf) for a full list of questions and answers from our COVID-19 and COPD webinar.
We are also aware of multiple media reports suggesting there is a shortage of albuterol inhalers. We are monitoring the situation and to date have seen no confirmation from manufacturers that there is an urgent issue. We will continue to monitor for potential supply chain issues but as a reminder, if you do encounter a situation where your pharmacy doesn’t have your medications in stock, check with your doctor regarding the specific medication and if alternatives are available. There is no single answer to whether you can reduce your inhaler dose or frequency – some medications have longer lasting effects than others and some people need higher doses than others. Don’t forget to keep up with your COPD management plans and check in on COPD360social to let us know how you are doing.
Should you use a nebulizer if you contract COVID-19? Why could it increase infection?
There is some concern that nebulizers used by those infected by COVID 19 could increase risk of aerosolizing the virus and infecting others in the surrounding area. An aerosolized virus potentially could stay in the air for 3-4 hours, much longer than the droplets we sneeze or cough into the air.
While there is the option of avoiding nebulizer use and switching to an inhaler regimen during this present COVID 19 epidemic, medical regimens should never be changed without discussing with your health care provider. Furthermore, for some with more severe disease or those who do not have the ability to successfully use an inhaler regimen, nebulizers may still be the preferred option. For those who need their nebulizer but understandably want to limit risk to those around them your provider could recommend a PARI filter for use with nebulizers that is reportedly equivalent to an N95 mask.
Updates from March 27, 2020plus
COVID-19 Policy Issues and What the COPD Foundation is Doing
At a time of immediate crisis, policy issues might be far from the top of your mind, but nonetheless, there is important work going on here in DC that could impact how we deal with the crisis and what resources are available to support our community. With that in mind, I want to take a moment to fill you in on what the COPD Foundation has been doing to bring your voice into these conversations and what we can expect in the coming days and weeks.
Our advocacy efforts are focused first on issues that could directly impact people with COPD as a result of the COVID-19 pandemic, but we are also joining with our patient and healthcare professional partners on broader issues central to our country’s response to COVID-19. The COPD Foundation is committed to making sure your voices are heard as the nation continues to deliberate how best to respond.
Here are a few highlights of recent issues we have weighed in on with Congress and with the Centers for Medicare and Medicaid Services (CMS). Do you see issues that you feel like are not represented in this list and that are likely to have an impact on your life and community as a result of COVID-19? Please speak up, share your concerns and discuss how we can all mutually support each other so we can carry your voices to policymakers here in DC.
Waivers: In a time of emergency, CMS can issue waivers that change their rules temporarily. Sometimes these waivers are mandated by Congress through legislation. Waivers issued by CMS technically only apply to people in Medicare and sometimes Medicaid, but in many cases, they set the tone for what private commercial insurance companies will decide to do as well.
Oxygen: We joined with patient and professional groups to ask CMS to issue a waiver to remove the requirements for in-person certification and recertification visits for someone on oxygen therapy. We also asked that they clarify they will accept other proof of delivery methods rather than signature as is currently required. We do not want people on oxygen to risk exposure to COVID-19 for these routine certification appointments and would prefer fully contactless delivery of oxygen equipment.
Home Infusions: People with alpha-1 antitrypsin deficiency-related COPD rely on a weekly infusion of augmentation therapy as a vital part of their treatment regimen. Currently, Medicare only covers augmentation therapy when it is given in a healthcare setting like an infusion center or hospital clinic, even though it can be safely administered at home by trained professionals. We urged Congress to include a waiver that will allow people with Alpha-1 and others who use infused therapies in Medicare to avoid unnecessary exposure and get their treatments at home.
Telehealth and Respiratory Therapists: We joined with the U.S. COPD Coalition partners in asking for a waiver to allow respiratory therapists to provide COPD management services via telehealth during the health emergency. We also supported the policies included in the first COVID-19 related legislation to ease restrictions on where and how telehealth services are provided. The time is now to unleash the power of telehealth to allow you to keep up with your COPD management while avoiding COVID-19 exposure. Respiratory therapists are well qualified to provide many important education and management services.
Cost and Coverage Related Issues: There has been a lot of coverage in the media about making COVID-19 testing free, but there are other concerns that require CMS and Congress to act to protect people from burdensome unexpected out of pocket costs and from losing access to their routine treatments.
90-Day Medication Supply: We joined group calls for Congress to require insurance companies, including Medicare Part D plans, to authorize a one-time 90-day refill of medications to minimize trips to the pharmacy. We also hope that this is done in a way that limits out of pocket costs, especially for those who are still within their plan’s deductible.
Formulary Restrictions and the Supply Chain: The patient advocacy community is also paying close attention to any potential issues with medication supplies and urged Congress to clarify that insurance companies must waive restrictive formulary requirements and allow patients to access any available equivalent medications if shortages of particular brands arise in the coming months. We also supported closer monitoring of supply chain issues by the FDA so we can be prepared to address any issues proactively.
Coverage: A time of national health emergency is not a time to lose or be without health insurance, so we advocated for numerous coverage-related policies like special enrollment periods to allow uninsured to enroll in eligible plans, protection of Medicaid benefits and others.
Nonprofit Relief Issues: We understand that people are facing extreme economic consequences and some of these same forces are affecting the nonprofit community now and likely into the remainder of the year. The National Health Council, an association lead by patient advocacy organizations, is leading efforts, along with other non-health related nonprofits, to ensure economic relief legislation that Congress passes incorporates the needs of nonprofits who are serving their communities in this time of need. In particular, we joined the calls to advocate that tax deductions for charitable giving be eligible for deductions even if people don’t itemize and to make nonprofits eligible to apply for small business grants and loan programs if they have faced economic hardships from COVID-19 related demands.
There are so many moving pieces of our country’s response to COVID-19, but these are just a few of the issues we felt strongly about. We will keep you posted as things evolve and do speak up if there is an issue affecting you or your community that might not be reflected yet in current COVID-19 related advocacy efforts.
Updates from March 24, 2020plus
On March 17, 2020 the COPD Foundation hosted the webinar, "COVID-19, COPD and You: Important Strategies from Leading Medical Experts on Managing Your Health." We received over 100 questions before and during the webinar and have worked with Dr. Byron Thomashow, Chief Medical Officer of the COPD Foundation and Dr. Barbara Yawn, Consultant to the COPD Foundation to provide as many answers as possible. You can access the Q and A document now on our coronavirus page under the webinar details. If you have questions that have not been answered here in the blog or in the webinar Q and A, leave a comment and we will do our best to get you timely answers where they exist.
Updates from March 20, 2020plus
We are working to get you answers to the questions submitted on the webinar Tuesday as quickly as possible. We had an incredible turnout and hundreds of questions so bear with us as we start rolling out the answers over the next few days.
If you are active on COPD360social, you know that a fun #FluffyFridays tradition developed when people started posting pictures of their pets as an uplifting break from the COPD discussion.
In this spirit, and after a week of offering advice about what NOT to do during the COVID-19 outbreak, let’s focus on ideas for what you CAN do. Here are some ideas to get the conversation started:
Some dos to keep you entertained and active in a time of COVID-19:
- Take a walk! Walking outside is safe, but still try to maintain a safe distance (ideally 6 feet) from others outside of your family as you walk.
- Enjoy a book, crossword puzzle or a meal from your front porch and chat with neighbors from a distance. I can vouch for this one-my six-year-old and I have mastered the art of long distance socializing by now and it might be saving our sanity!
- Learn an instrument. We are partial to harmonicas of course, but the options are endless. Check out online stores or call to see if the local music store is delivering and pick an inexpensive instrument with a “how-to” video on youtube. Our own Stephanie Williams is using her social distancing time to learn ukulele. Her first performance is live on COPD360social or at https://youtu.be/yPPJF4sX_2M.
- Check out any of these great free resources featured in Stephanie’s presentation on Tuesday’s webinar like free virtual museum tours, classes and more. Below are some resources for staying engaged.
- Challenge yourself to a pantry cooking game and see what fun recipes you can create using just what you have on hand. Snap a picture of your masterpiece and share with others right here on COPD360social.
- Start a social distancing journal, keep note of how you feel, what you are doing, exercises, medications taken, etc. The days may start to run together, so keeping notes on the day to day can help keep things on track.
Some do’s about COPD in a time of COVID-19: We are the COPD Foundation after all, so we can’t miss out on an opportunity to remind you about a few self-care must dos.
- Update your Action Plan. Take some time to revisit your COPD Action Plan and make sure it is still up to date and reflects the goals you have for COPD management. Make sure to send a copy to your healthcare professional and check-in with them virtually if you think changes are needed.
- Refresh your inhaler technique knowledge using our free online video library
- Practice pursed lip breathing several times a day
- Keep taking your maintenance medications routinely
- Keep moving. If you can’t get outside and walk, find ways to keep your body moving while indoors.
Updates from March 18, 2020plus
Updates from March 15, 2020plus
COVID-19, COPD and You: Important Strategies from Leading Medical Experts on Managing Your Health
The COPD Foundation wants you to know you are not alone during this time.
We will be hosting a webinar that will provide you with updated medical information about managing your chronic obstructive pulmonary disease during the COVID-19 (Coronavirus) pandemic.
This webinar will feature presentations by leading medical and public health experts from Johns Hopkins Medicine, the Johns Hopkins Bloomberg School of Public Health and Columbia University/New York-Presbyterian Hospital. During the webinar, these experts and COPD Foundation staff will address commonly asked questions about the virus and provide strategies and suggestions for living with COPD in the time of COVID-19.
Please join us to learn more. You can join with your computer, smartphone or tablet OR you can join to listen in through your phone but still need to register at the link below to receive the phone number.
Date: Tuesday, March 17th
Time: 6:00 pm ET
Registration: https://attendee.gotowebinar.com/register/6287160725295712267
Join us in learning how we can face this crisis together.
Updates from March 11, 2020plus
I have heard there is a shortage of test kits. Will people with COPD be able to get tested if we are concerned about symptoms?
At the present time there are limited supplies of test kits. The availability of test kits appears to be different by region but there is no one information source to show the exact shortages by state.
Eventually, most experts expect that test kit availability will improve and more people will be tested, but the progress has been slow. Since the CDC has said that people with lung disease are a high-risk population, it is our hope that anyone with COPD and symptoms of COVID-19, and those with symptoms who have close contact with COPD patients will be able to get testing in a prompt and safe fashion, especially in areas with known outbreaks.
How do we know the difference between a typical exacerbation (flare-up) and symptoms of COVID-19?
There is likely to be some overlap between the symptoms you normally experience during a COPD exacerbation or flare-up and symptoms of COVID-19. There is also no "typical" COPD exacerbation, since each individual experiences a range of mild to severe symptoms.
Early reports show that high fever is a common symptom of COVID-19, but in general, high-grade fevers are less likely to happen in a COPD exacerbation. You should pay particular attention to what your "normal" exacerbation symptoms are and reach out to your doctor if you are at all concerned about shortness of breath and any symptoms that may be different from your "everyday" of living with COPD, just as you would with typical COPD exacerbations. Most medical practices and hospitals are asking that you call first, rather than visiting the office or emergency room, unless it is a life-threatening situation.
How should I adjust my COPD Action Plan during the COVID-19 outbreak?
A COPD Action Plan is a great tool for preventing exacerbations and treating them early when they do occur. The My COPD Action Plan is one example; it is also available on the COPD Pocket Consultant Guide Application but if you have not already agreed on an action plan with your health care provider, it is important to contact them to complete it together.
If you already have a COPD action plan there may not be many differences related to COVID-19. The one exception to this is if you have agreed to start antibiotics and/or steroids upon early signs of exacerbation, you should consider reaching out to your doctor to see if they would suggest adding a phone consultation prior to starting the medication. As always, when in doubt, ask your doctor.
My loved one has COPD and lives in a senior facility/nursing home/assisted living and I have heard there is an increased risk in these places. What should I be asking the facility about their plans for people with respiratory disease?
The COVID-19 outbreak in a Washington nursing home raised concerns about the risks faced by others in similar places, including nursing homes, assisted living homes and other senior institutional living arrangements. Recommendations include very strict limits on visitors, flexible sick leave policies for workers, rules to identify and address sick workers, education and training on COVID-19 for residents and workers and a series of improved cleaning and infection-control practices.
If your facility hasn’t implemented visitor restrictions or other policies consistent with the CDC recommendations, you should ask them how they are planning to respond. Consider asking what arrangements they are making so there is enough oxygen and protective gear available, along with what policies they are putting in place so they can be sure higher-risk patients, like those with lung disease, are assessed and moved to a hospital if necessary. Finally, consider suggesting that they conduct additional outreach to the facility’s employees to educate them about lung disease and the early signs and symptoms of exacerbations. You can send them to the COPD Foundation’s website for downloadable resources or videos.
Updates from March 10, 2020plus
We appreciate all the great discussion occurring on COPD360social and on our social media pages. We will continue to address your questions here on the COPD Digest Blog and to follow the latest information from the CDC for people at higher-risk for COVID-19 complications.
Will I have to pay for COVID-19 related testing and services? Can I get an early refill or 90-day supply to prepare for the possibility of home isolation?
The answer depends on what type of insurance you have and what services are needed.
The COPD Foundation supports action from state and federal authorities to require all insurers to waive cost-sharing (the amount you have to pay) for COVID-19 testing AND related treatment. Some states have already started to act and declare all testing will be free to patients, but it should be universal. Today, a group of major insurance companies including UnitedHealth, Anthem, Blue Cross Blue Shield Association, Aetna and Cigna and Humana, met with President Trump and Vice President Pence and committed to ensuring cost would not be a barrier to COVID-19 testing, but the details on who this applies to and how it will be implemented are not known at this time, nor is it known how treatment related costs for positive cases will be handled. Cost should not be a barrier to good prevention practices and accessing early care if you are concerned you have symptoms of COVID-19.
Insurers should also take actions to make it easier for people to obtain a one-time early refill or longer supplies of their medications to prepare for possible home isolation, especially for high-risk populations. Telehealth services should be encouraged and reimbursed to give high-risk patients more options to avoid missing scheduled appointments.
If you would like more information about coverage for COVID-19 related testing and treatment, or coverage for backup supplies of your medications, here are a few places you can reference to find out more depending on what type of coverage you have.
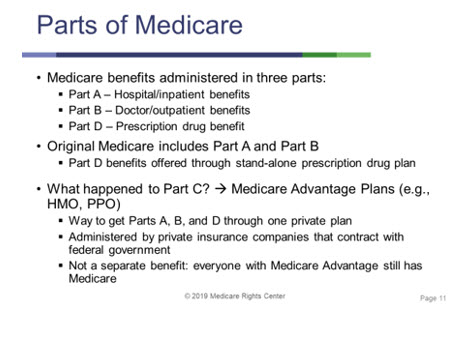
Here is a reminder from our October webinar with our partners at the Medicare Rights Center about the services each part of Medicare covers to help guide your outreach if necessary. We will continue to follow developments related to the cost and access to testing and treatment for COVID-19 and encourage you to share your experiences. Have you heard directly from your healthcare professionals or their institutions? How are they communicating with you about the risks in your community and what action they are taking to ensure you can access the care you need for your COPD management and if necessary, for COVID-19 testing and treatment?
Can I catch COVID-19 from packages like mail or grocery bags?
Yes, but it is very unlikely. The CDC explains why in their Q and A at https://www.cdc.gov/coronavirus/2019-ncov/faq.html#spreads. Extra precautions can't hurt, even if the risk is low. Washing your hands or if that isn’t possible, using hand sanitizer makes sense after touching surfaces or handling objects that others may have been touching.
"It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads. In general, because of poor survivability of these coronaviruses on surfaces, there is likely very low risk of spread from food products or packaging that are shipped over a period of days or weeks at ambient, refrigerated, or frozen temperatures."
Updates from March 9, 2020plus
In the last update, we reported that CDC had changed their recommendations to suggest that people in the high-risk categories should consider staying home as much as possible. Over the weekend their suggestions were revised once again to include a caveat that this should be a consideration "during a COVID-19 outbreak in your community". So, what does this mean for people with COPD now that over half of the states in the U.S. have reported a confirmed case?
There is no one right answer to how much you should travel outside your home right now, but we can suggest a few questions that you can walk through to guide your decisions. When in doubt, reach out to your doctor!
Questions to guide your decision making:
- How important is the activity or travel outside of your home?
-
What is the status of the COVID-19 outbreak in your community?
Are there confirmed cases in your state, how many and can they be traced to a known exposure or is the source of the infection unknown (community spread)? We recommend you check the website for your state and/or local health departments for this information and to view state and local advice about limiting your time outside of your home. This website provides updated information on where cases are in the United States.
-
How great is my health risk category?
Even though about 80% of COVID-19 cases are considered mild, early data is showing COVID-19’s effects are worse for older adults (likely over 60) and people with heart and lung disease or diabetes. Consider the risks faced by those you live with or take care of as part of your calculation.
-
If you are considering traveling away from home: Am I prepared if travel disruptions or required quarantines require me to stay at another destination for a prolonged period?
CDC is now recommending that people in the high-risk category avoid non-essential travel, but particularly long plane flights and cruises. Consider updated travel information at https://www.cdc.gov/coronavirus/2019-ncov/travelers/index.html.
Updated CDC Recommendations for High-Risk Populations:
Extracted from the CDC on March 8, 2020
If you are at higher risk of getting very sick from COVID-19, you should:
- Stock up on supplies.
- Take everyday precautions to keep space between yourself and others.
- When you go out in public, keep away from others who are sick, limit close contact and wash your hands often.
- Avoid crowds as much as possible.
- Avoid cruise travel and non-essential air travel.
- During a COVID-19 outbreak in your community, stay home as much as possible to further reduce your risk of being exposed.
Updates from March 7, 2020plus
The CDC has updated its recommendations for people at higher risk of experiencing complications from COVID-19, including people with lung diseases like COPD. As the disease is detected in more states, it is important for people with COPD not to panic, but to prepare and take steps to minimize your risk of exposure such as limiting public activities. As always, if you have questions about your individual circumstances we encourage you to reach out to your doctor directly. The core CDC recommendations are included below. Visit their page for older adults and high-risk populations to learn more about preparation and support that might be available in your communities. We will continue to monitor the situation and share updates relevant to the COPD community.
CDC Recommendations: What to do if you are at higher risk:
- Stay at home as much as possible.
- Make sure you have access to several weeks of medications and supplies in case you need to stay home for prolonged periods of time.
- When you go out in public, keep away from others who are sick, limit close contact and wash your hands often.
- Avoid crowds.
- Stay up to date on CDC Travel Health Notices.
Updates from March 6, 2020
What are the best resources to help teach my family good handwashing technique?
Make sure you are washing your hands correctly with this thorough tutorial from the World Health Organization (WHO). Print a few out and hang them near sinks. https://www.who.int/gpsc/clean_hands_protection/en/. Prefer video? Check out this WHO video tutorial. https://www.youtube.com/watch?v=3PmVJQUCm4E
Can I make my own hand sanitizer?
Proper handwashing is always the preferred practice. When that isn't possible, many with COPD regularly use an alcohol-based hand sanitizer. We know there is a nationwide shortage of sanitizer and many have suggested recipes for making your own. While this can be effective, it is a BIG IF because you must follow the instructions carefully and end up with a sanitizer that has at least 60% alcohol. You should also consider the risks of accidental ingestion or contact with the alcohol if you have children in your household and use it only as a last option if no soap and water, antibacterial wipes or commercial sanitizer are available.
Updates from March 5, 2020plus
As information continues to evolve on COVID-19, we have received some additional questions and have worked with our medical advisors to provide the following answers. Thank you to our COPD360social community for supporting each other and engaging in a positive and fact-based dialogue about what the community can do to prevent COVID-19. As a reminder, the CDC website at https://www.cdc.gov/coronavirus/2019-ncov/index.html is the most comprehensive source of information about COVID-19.
Should I cancel my routine doctor’s appointments or screenings to avoid exposure to medical facilities?
There is no one answer to this question as it depends on your unique circumstances, but here are a few things to consider:
- First and foremost, if you are concerned talk to your doctor and explain your concerns. Ask if they feel comfortable with you delaying your appointments.
- Assess the current situation in your state and local community. As of March 4, COVID-19 has been reported in 13 states, with most states, other than California, Washington and Oregon, only having a small number of confirmed cases. Consider your risk before making any decisions. If there has not been confirmed community spread of COVID-19 in your community, your risk is still low and delaying medical appointments can carry risk in itself.
- If you are in an area where there has been documented community spread and you are concerned, ask your doctor about the possibility of virtual visits. Many practices have added telehealth options to their services for select issues and they may consider offering to consult with you via their telehealth platform, often an app or a website that can be used on a smartphone, tablet or camera-enabled computer.
Why does the media keep suggesting that we get flu and pneumonia vaccines when they don’t protect against COVID-19?
While the flu shot and the two pneumonia vaccines do not specifically prevent contracting COVID-19, they do help prevent potentially complicating conditions like the flu and pneumonia and widespread infection from a specific type of bacteria-the pneumococcal group. If you did contract COVID-19, being up to date on both vaccines would reduce your risks of contracting flu and pneumonia at a time that your health is already compromised. It is not too late to have an annual flu shot and people with COPD should have both the Prevnar 13 and the pnuemovax shots. Typically, there is a one-year window between the two, however, you can check with your doctor to see if your underlying health condition means you should receive the second shot sooner than a year. In most cases, both vaccines should be covered without cost to you.
Will contracting COVID-19 make my COPD worse in the long-term?
There is not enough evidence specific to COVID-19 to predict how it will affect the long-term lung function and disease trajectory for people with COPD. All we can do is look at what we know about exacerbations/respiratory infections in general. We focus on helping patients avoid exacerbations and address them early when they do occur. One suggestion is to have a written action plan with your physician. You can complete one on our app or print one out and share it with your physician.
We know it’s tough to balance being cautious and taking preventive steps to reduce the likelihood you get sick from COVID-19, the flu or pneumonia with going about your daily life and doing the activities that you want and need to. Our best advice is to share your concerns with your doctor, do the things you know help prevent infections and stay up to date with the evolving information on the risk in your community.
Updates from March 3, 2020plus
As the COVID-19 situation continues to evolve, more information is emerging about the disease and what you can do to help protect yourself.
Please find below some Q&A that address some important factors.
What is COVID-19?
COVID-19 is a new disease caused by a novel coronavirus that is different than the common cold, flu or pneumonia. COVID-19 emerged in China in late 2019 and is now present in multiple other countries, including the U.S.
What are the symptoms of COVID-19?
Symptoms of COVID-19 are like those of a respiratory infection, including fever, cough, and shortness of breath. The disease is spread primarily through person-to-person contact and contact with respiratory droplets from the sneeze or cough of an infected person, however, it is possible but less likely, that people who don’t have symptoms could spread the disease.
Is the coronavirus/COVID-19 present in the U.S.?
The first case of “community-spread,” of COVID-19 in the United States was reported on February 26, 2020. The virus has been confirmed in numerous states in the U.S. and it is expected that additional cases will continue to be identified in the U.S.
What is the risk of contracting COVID-19 for people with COPD?
Despite the increase in cases, the risk of contracting coronavirus is still low in the U.S. However, people with COPD and other lung conditions are at increased risk of severe outcomes if they do contract COVID-19, just as is the case with typical respiratory infections, the seasonal flu, and pneumonia. If you have reason to suspect you might have any type of respiratory infection, prompt action is critical. Get further tips for actions to take if you have early warning signs of an exacerbation.
What should people with COPD do to prepare for COVID-19 or the potential of voluntary home isolation?
- Take basic preparedness steps to ensure you have the supplies you would need to allow you to stay home comfortably should you need to avoid public places in the future. These steps are similar to what you would do to prepare for an emergency like an earthquake or hurricane. You can read about general preparedness in our guide at:
- Refill your medications if possible, so that you have at least a 30-day supply on hand. If your insurance allows for 90-day supplies, then request this the next time you refill.
- Call your oxygen supplier and ask if they are making plans to prepare for a coronavirus outbreak in your community.
- If you rely on visiting nurses or aids to help you with household tasks, ask if they have plans for ensuring appropriate prevention practices.
What should I do if the pharmacy runs out of my COPD medications and I can’t locate them at another pharmacy?
Check with your doctor regarding the specific medication and if alternatives are available. There is no single answer to whether you can reduce your inhaler dose or frequency – some medications have longer lasting effects than others and some people need higher doses than others.
Updates from February 28, 2020plus
We understand the COPD community may have questions about the coronavirus, now called COVID-19. We want to reinforce that the most important thing people with COPD can do is prevent the spread of respiratory infections with a few simple practices. If you have specific concerns about your individual health circumstances, we encourage you to contact your healthcare professional team directly.
To prevent the spread of respiratory infections following a few simple suggestions may help.
- Avoid being close to people who have a respiratory infection like a cold or influenza
- Consider switching from handshakes to elbow bump
- Wash hands often
- When you cannot wash your hands, consider using a hand sanitizer
- If you have a respiratory infection, stay home from activities where you may spread the infection-- church, schools, sporting or social events
- Cover your nose and mouth if you are coughing from a respiratory infection and help others around to learn to do the same
The CDC has updated its travel warnings. You should avoid nonessential travel to China and South Korea, and consider postponing travel to Italy, Iran, and Japan. For countries outside of this list, please speak directly to your health care team and regularly monitor the CDC site at https://www.cdc.gov/coronavirus/2019-ncov/travelers/index.html for updated warnings if you are considering international travel.
Many in the community have asked what they can do to prepare for the possibility that coronavirus becomes more widespread in the United States. While there is no evidence that there is an imminent threat, general preparation steps can be taken so that you are able to spend an extended amount of time at home if necessary. These steps are similar to what you would do to prepare for an emergency like an earthquake or hurricane.
You can read about general preparedness in our guide at:
Here are a few additional steps you might want to consider taking.
- Refill your medications if possible, so that you have at least a 30-day supply on hand. If your insurance allows for 90-day supplies, then request this the next time you refill.
- Call your oxygen supplier and ask if they are making plans to prepare for a coronavirus outbreak in your community.
- If you rely on visiting nurses or aids to help you with household tasks, ask if they have plans for ensuring appropriate prevention practices.
What should people with COPD do to prevent from contracting COVID-19?
The most important thing people with COPD can do is to practice good infection control practices as you would to prevent any respiratory infection.
- Handwashing is key. Make sure you follow best practices for handwashing at https://www.cdc.gov/handwashing/when-how-handwashing.html
- When you cannot wash your hands, consider using a hand sanitizer with a high alcohol content
- Avoid being close to people who have a respiratory infection like a cold or influenza
- Consider switching from handshakes to elbow bump
- If you have a respiratory infection, stay home from activities where you may spread the infection-- church, schools, sporting or social events
- Cough into your elbow or directly into a tissue if you are coughing from a respiratory infection and help others around to learn to do the same
- Practice good general nutrition habits to ensure your immune system is as strong as possible
Should people with COPD wear masks in public?
There are two types of masks commonly mentioned in media coverage, the surgical mask, and the N95 mask. NEITHER mask is recommended for the prevention of respiratory infections. Furthermore, the N95 mask can be tough for people with COPD to use, and in some patients, prolonged use of the N95 mask can cause more shortness of breath, lower blood oxygen saturation and higher exhaled carbon dioxide levels.
Both types of masks are currently in short supply and health officials are urging the public to refrain from buying supplies of masks that are critical for the healthcare workers taking care of infectious diseases of all types to access. If you would like to discuss your questions about masks further, we encourage you to reach out directly to your healthcare professional team as they will be best suited to evaluate your unique circumstances.
Read the latest information on COVID-19 from the CDC at https://www.cdc.gov/coronavirus/2019-ncov/index.html.