What does it mean when COPD symptoms are controlled? Part 1
Posted on December 03, 2019 |
This post was authored by Barbara Yawn, MD, MSc, FAAFP of the University of Minnesota; M. Bradley Drummond, MD of the University of North Carolina at Chapel Hill School of Medicine; and Carol Rubin, MEd, MS of Cliffside Park, NJ.
Chronic obstructive pulmonary disease (COPD) is not a single condition1 but includes emphysema (damage to the air sacs of the lung) and chronic bronchitis (chronic cough with mucus production caused by inflammation of the breathing tubes) and leads to shortness of breath.2 Symptoms of COPD vary from person to person and from day to day or by the time of day3 and can include difficulty in breathing (shortness of breath), increased mucus, frequent coughing, chest tightness, and wheezing (whistling sound) when breathing out.2
What does it mean when your COPD symptoms are controlled?
Symptoms are considered under control, or stable, when they are about the same day to day, and allow you to do what is normal for you—functioning at your best.2 Understanding what is “normal” for you—meaning when symptoms are under good control—can be assessed by following your day-to-day symptoms using the COPD Foundation patient app.4 (Suggested reading: The COPD Pocket Consultant Guide Mobile App) Knowing what is normal can help you and your doctor or nurse decide when you are in control or when things are getting worse or out of control. This helps you know if a visit is needed to receive more or different treatments. (See our upcoming post What does it mean when COPD symptoms are “controlled”? Part 2 for more information about baseline COPD symptoms and how to improve your ‘normal.')
You should visit your doctor or nurse on a regular basis. At these visits you should review symptoms, medications, inhaler technique, and talk about how well your treatment is working.2 You can also discuss any factors that may be making your symptoms worse and assess your lung function with spirometry when needed. (See our upcoming post Diagnostic decisions: What is spirometry and why is it important? for more information about spirometry.) A quick questionnaire like the COPD Assessment Test (CAT)2,5 can give you and your doctor or nurse important information about how you are doing and can be followed over time using the COPD Foundation app.
What should you do if your COPD symptoms are controlled?
First, understand why your symptoms are controlled—because you are likely doing things right such as taking your medication(s) every day, using good inhaler technique, working to avoid triggers like smoke or air pollution (or other things you know will make your symptoms worse), and trying to include some physical activity everyday.2 COPD is a chronic illness that you will have for the rest of your life.2 Therefore, continue taking your medications every day, even if your symptoms are controlled or it is a really good day.
What happens when your COPD symptoms are not controlled?
You may experience a sudden worsening of symptoms known as a flare-up or acute exacerbation2, which reflects a change from green to yellow or red days on the COPD Foundation app.6 When this happens, you should talk to your doctor or nurse. Remember that several things can get your symptoms “out of control” including chest infections like colds or bronchitis, large temperature changes, smoke, indoor/outdoor pollutants, dust, pet dander, strong odors (e.g., perfumes), or pollens.2 Contact your doctor or nurse when:2,6
- Your cough, wheeze, or shortness of breath is worse than your ‘“normal”
- You have more mucus, or it changes color or is thicker
You need to seek immediate attention such as going to the emergency department or call 911 if you:
- Are coughing up blood
- Have chest pain, blue lips and/or fingers, fever and lack of mental alertness, or swollen feet or ankles
- Experience severe shortness of breath or chest tightness or worsening despite your usual treatments
What can you do to keep your COPD symptoms controlled?
- Work with your doctor or nurse to make a personalized COPD action plan. Try the one from the COPD Foundation (Figure 1),6 using the COPD Foundation patient app. The app allows you to track your COPD action plan and share the progress with your doctor (Figure 2).
- Follow the action plan—take your medications as directed, use correct inhaler technique, be on the look-out for early warning signs, and act fast when symptoms worsen.
- Use your action plan to meet your needs, set goals, and share how you have been doing with your clinician.
While you and your clinician are making your COPD action plan, ask questions such as:
- What are early warning signs my symptoms are becoming uncontrolled?
- What medication should I take to when my symptoms get worse?
- When should I call the office or go the emergency room?
- How do I know if I am using my inhaler correctly?
Use the COPD Foundation app to see a list of questions to ask your doctor. The app also contains instruction videos on how to correctly use your inhaler. Also, avoid triggers, participate in a pulmonary rehabilitation program, and be up to date with vaccinations (Suggested reading: National Immunization Awareness Month.
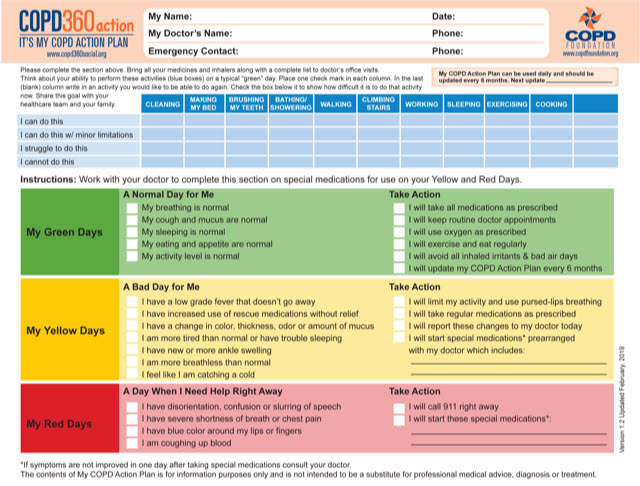
Figure 1. The COPD Foundation My COPD Action Plan.6
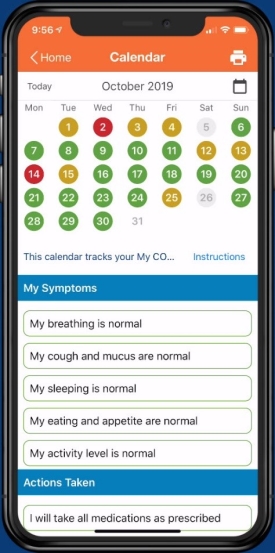
Figure 2. A person with COPD tracking the action plan on the phone over a period of one month.
During each office visit, remember to:
- Update and review your action plan, and discuss what you can and cannot do
- Have your medications with you, and get your inhaler technique checked
- Get vaccinated when needed
- If you are smoking, ask about ways to get support including medicines to help stop
Please see the accompanying infographic for information about COPD symptoms, triggers, and impact on daily living.
Download Infographic
Acknowledgments
The authors meet the criteria for authorship recommended by the International Committee of Medical Journal Editors. The authors received no direct compensation for the development of this manuscript. Writing, editorial support, and formatting assistance was provided by Praveen Kaul, PhD, Frances Gambling, BA (Hons), and Maribeth Bogush, PhD of Cactus Communications, which was contracted and compensated by Boehringer Ingelheim Pharmaceuticals, Inc., (BIPI) for these services. BIPI was given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Disclosures
Dr. Yawn reports personal fees from Boehringer Ingelheim, AstraZeneca, GlaxoSmithKline, and Midmark, and grants from the COPD Foundation, Boehringer Ingelheim, and the National Heart, Lung, and Blood Institute (NHLBI) outside the submitted work.
Dr. Drummond reports grants from the NHLBI, the U.S. Department of Defense, and Boehringer Ingelheim outside the submitted work. He also reports personal fees from Boehringer Ingelheim, GlaxoSmithKline, AstraZeneca, Mylan-Theravance, Novavax, Parion, Midmark, and Philips outside the submitted work.
Ms. Rubin reports personal fees from Novartis and the U.S. Department of Defense outside the submitted work. She is associated with the COPD Foundation as a State Captain, which is a non-paid position.
References
- World Health Organization (WHO). Chronic obstructive pulmonary disease (COPD). 2019. Retrieved from https://www.who.int/health-topics/chronic-respiratory-diseases#tab=tab_1. Accessed: November 11 2019
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2020 Report. Retrieved from https://goldcopd.org/ Accessed: November 11, 2019.
- Lopez-Campos JL, Calero C, Quintana-Gallego E. Symptom variability in COPD: a narrative review. Int J Chron Obstruct Pulmon Dis. 2013; 8:231-8.
- Thomashow B, Crapo JD, Drummond MB, et al. Introducing the new COPD pocket consultant guide app: can a digital approach improve care? a statement of the COPD foundation. Chronic Obstr Pulm Dis. 2019; 6:210-20.
- The COPD Assessment Test (CAT) website for members of the public. 2018. Retrieved from https://www.catestonline.org/. Accessed: November 11, 2019
- The COPD Foundation. My COPD Action Plan. Retrieved from https://www.copdfoundation.org/Downloads/MyCOPDActionPlan.pdf. Accessed: November 11, 2019.