Oct 2015 PRAXIS Resource of the Month – The COPD Action Plan
Posted on October 01, 2015 |
This post was written by Kristen Willard, M.S.
Research has shown that clear action plans may improve health outcomes for people with COPD. One 2011 study showed that adherence to an action plan was associated with more prompt treatment and therefore a reduced exacerbation recovery time; an earlier study revealed that those employing a COPD action plan as part of their care were significantly less likely to require hospitalization than were their standard of care counterparts.
How might COPD action plans improve COPD care?
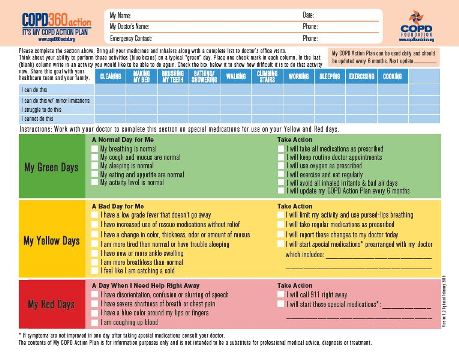
Improved communication – The physical action plan document is a tool that, when used by patients and their entire care team, ensures each member of the group is speaking the same language. That is, when a patient determines he is having a "yellow" day, as evidenced by a set of symptoms specific to him, both he and his healthcare provider have a clear understanding of what that means and what their expected next steps will be.
Establishes the patient as a partner in care – No one knows a patient's experience better than they do. The COPD action plan helps those with COPD to monitor more closely changes in their own bodies and how they can self-manage those changes. It empowers the patient to be an active participant in their care as they learn to recognize what triggers flare-ups and understand that, if necessary, their healthcare team will respond in an established manner.
Improved efficiency – In a well-executed action plan, the healthcare provider will know that a patient has tried all agreed upon at-home care prior to reaching out for support. This can result in more efficient decision making on the part of a provider about the need for more intensive follow up for their patient.
Barriers to potential use:
Time – The implementation of action plans requires time on the part of one or more care team members to ensure that the plan is 1) tailored to the specific patient in a way that is useful and 2) communicated effectively to that patient.
Tips:
Customization – Customization is key given that there is not a single COPD road map traveled by all patients. Action plans should be tailored to include an individual’s specific situation, including triggers, medications and baseline symptoms.
Distribution – Once an action plan is customized and discussed, copies should be distributed to all health care team members.
Living document – The COPD action plan is an evolving document. If a patient's situation, medication or treatment approach changes, the plan should be updated to reflect those changes.
The COPD action plan found in PDF form below is used by Crouse Hospital in Syracuse, NY (https://www.crouse.org/). The COPD Foundation has produced its own plan (see right) called the My COPD Action Plan (see right); it can be found here!
Let us know in the comments: What are your thoughts on this as a tool to improve COPD care and the patient experience? Does your team use COPD action plans in your work? If you'd like, please share your approach in the comments.
This page was reviewed on March 6, 2020 by the COPD Foundation Content Review and Evaluation Committee