This article was written by Jane Martin, BA, RCP
This is the second in a series of four blog posts on NTM lung disease.
In our first blog post we learned about nontuberculous mycobacteria (NTM) and the disease it causes, NTM lung disease. Like COPD, NTM lung disease is a chronic, progressive disease that makes it hard to breathe. Common symptoms of NTM lung disease are shortness of breath, fever, weight loss, chronic cough, fatigue, and chest pain.i Some of these symptoms can also be found in COPD, bronchiectasis, and asthma, the very conditions that increase the risk for getting NTM lung disease.ii This increased risk exists because damage from these conditions can make it easier for NTM bacteria to infect the lungs. All of this can make diagnosing NTM lung disease complex.
Sometimes this challenge may cause a delay in diagnosis and treatment. Untreated symptoms can get worse and cause more damage to the lungs. This means that a delay in the diagnosis of NTM lung disease can make the condition worse.iii Even so, the good news is that NTM lung disease can be successfully diagnosed and that treatment options are available.
Some locations have higher rates of NTM lung disease
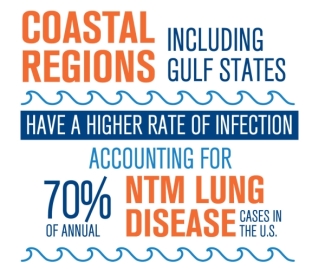
Figure 1 citation: Strollo SE, Adjemian J, Adjemian MK, Prevots DR. The burden of pulmonary nontuberculous mycobacterial disease in the United States. Ann Am Thorac Soc. 2015;12(10):1458-1464.
When considering diagnosis, a variety of factors must be taken into account, including physical symptoms and test results. Another of these factors is geographic location – where the person lives. Some geographic areas tend to have higher rates of NTM lung disease. Coastal areas, including Gulf states, have a higher rate of infection, accounting for 70% of annual NTM lung disease cases in the U.S.iv
As well as these coastal regions, there are seven large clusters with a higher risk of NTM lung disease. These areas are found in 55 counties in eight states, including parts of California, Florida, Hawaii, Louisiana, New York, Oklahoma, Pennsylvania, and Wisconsin.v
How is NTM lung disease diagnosed?
Now let’s see how healthcare providers test for NTM lung disease. Medical diagnosis is based on findings in three main areas. Each one of these plays a role in helping a healthcare provider find out if a person has NTM lung disease.i
- Reviewing medical history and doing a physical exam
- Radiographic imaging
- Sputum (mucus) testing
Let’s take a closer look at each of these.
History and physical – The healthcare provider asks the patient questions about their medical history, symptoms, and other aspects of everyday life. He or she also performs a physical examination.
Radiographic imaging – X-ray-type testing is done followed by careful analysis of the images by a radiologist (a doctor trained in reading x-rays). A high-resolution CT (computed tomography) scan is commonly used and can show much more detail than a regular chest x-ray.
Testing sputum (mucus) samples – NTM bacteria is found in sputum, or mucus. Multiple samples taken early in the morning, on different days, are collected in special cups. A good sample is not just saliva, the wet substance in your mouth. For this test, mucus coughed up out of the lungs is needed. If a person cannot cough up enough sputum, it may be necessary to get a sample by doing a bronchoscopy or a biopsy.
Testing for NTM bacteria takes longer than a simple test checking for a routine infection. It is possible for laboratory testing to be complete within two to three weeks, but it can take from eight to 12 weeks.vi
One patient’s experience with diagnosis of NTM lung disease
We know that COPD is not a one-size-fits-all disease. Symptoms and the impact they have on daily life can vary widely from person to person. Likewise, different people have different experiences with diagnosis. It is the same with NTM lung disease.
Here is part of one person’s experience with her diagnosis of NTM lung disease.*
My first symptom was a cough in September of 2001. But the big thing was fatigue. I was so tired all the time, I just couldn’t function. I was barely able to get through my day. Just walking up a flight of stairs was a problem, when not long before that I could exercise, do yoga, and walk up to three miles.
Later that month, my doctor prescribed antibiotics. He also ordered a chest x-ray that didn’t show anything. Over the next few months the symptoms continued, but I went on with my life. I traveled to China to adopt a child! Despite a constant cough, increasing fatigue, and a frequent, low-grade fever, I was in denial that this could be a serious illness.
But as the months went by, I came to realize that it was serious. By April, I knew that there was something really wrong with me. At that time, doctors weren’t very aware of NTM lung disease (but education and awareness is helping that now), so I pressed my primary care doctor to order a pulmonary function test. The test was abnormal. In June, as a follow-up to the abnormal pulmonary function test, I had a CT (computed tomography) scan. Later that summer my mucus was tested for NTM.
By that September, one year after noticing my first symptoms, I had lost 30 pounds. At the end of that year, fifteen months after first having symptoms, it was confirmed that I had NTM lung disease. My treatment was started the next month, in January.
*Please note that this is just one person’s experience of being diagnosed with NTM lung disease. Each patient, situation, and diagnosis story is unique.
Summary
NTM lung disease can be complicated and challenging to diagnose. But increased awareness and education may help make diagnosis easier and more commonplace. Paying attention to symptoms and reporting them to a healthcare provider is important. Earlier NTM lung disease diagnosis and successful treatment may help slow the rate of lung function decline.iii
When diagnosis is confirmed, the healthcare provider and patient should talk together about what comes next. Going over the potential risks and benefits of therapy is key, always keeping in mind the value of patient-centered care and quality of life.vii
In our next blog post we will look at day-to-day living with NTM lung disease and treatment.
Thank you to Katie Keating, RN, MS, for sharing her story.
This blog post is sponsored by Insmed Incorporated.
References
i Young JD, Balagopal A, Reddy NS, Schlesinger LS. Differentiating colonization from infection can be difficult. Nontuberculous mycobacterial infections: Diagnosis and treatment. J Respir Dis. 2007;28(1):7-18.
ii Andréjak C, Nielsen R, Thomson VO, et al. Chronic respiratory disease, inhaled corticosteroids and risk of nontuberculous mycobacteriosis. Thorax. 2013;68(3):256-262.
iii Mirsaeidi M, Hadid W, Ericsoussi B, Rodgers D, Sadikot RT. Non-tuberculous mycobacterial disease is common in patients with non-cystic fibrosis bronchiectasis. Int J Infect Dis. 2013;17(11):e1000-e1004.
iv Strollo SE, Adjemian J, Adjemian MK, Prevots DR. The burden of pulmonary nontuberculous mycobacterial disease in the United States. Ann Am Thorac Soc. 2015;12(10):1458-1464.
v Adjemian J, Olivier KN, Seitz AE, Falkinham III JO, Holland SM, Prevots DR. Spatial clusters of nontuberculous mycobacterial lung disease in the United States. Am J Respir Crit Care Med. 2012;186(6):553-558.
vi Griffith DE, Aksamit T, Brown-Elliott BA, et al; for the ATS Mycobacterial Diseases Subcommittee. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367-416.
vii Ryu YJ, Koh WJ, Daley CL. Diagnosis and Treatment of Nontuberculous Mycobacterial Lung Disease: Clinicians’ Perspectives. Tuberc Respir Dis (Seoul). 2016;79(2):74-84.