Why is it important to use your COPD inhalers correctly and regularly?
Posted on January 29, 2020 |
This post was authored by Barbara Yawn, MD, MSc, FAAFP of the University of Minnesota; M. Bradley Drummond, MD of the University of North Carolina at Chapel Hill School of Medicine; and Carol Rubin, MEd, MS of Cliffside Park, NJ.
Regular and correct use of inhaled medicines helps control symptoms of chronic obstructive pulmonary disease (COPD). However, your medicines will only work if you use your inhaler properly. Correct inhaler use makes sure that the right amount of medicine reaches your lungs. However, many different types of inhalers are available, and each requires a different technique. It is helpful if your doctor or a medical professional shows you how to use the inhaler prescribed to you.
What is meant by proper inhaler technique?
Your ability to use your inhaler properly, with the correct breathing technique, can affect your lung health.1 This is referred to as “inhaler technique” and can differ from inhaler to inhaler. Using the wrong inhaler technique means that less medicine reaches your lungs.1,2 This can make you feel worse and put you at a greater risk of hospitalization.1 There are two main ways to take your inhaled medicine—using an inhaler or a nebulizer. Inhalers are small devices that can be held in your hand and are easy to carry.3 Three basic types of inhalers are available—a pressurized metered-dose inhaler (pMDI), a dry-powder inhaler (DPI), and a slow-/soft-mist inhaler (SMI).3 Nebulizers are machines that are usually larger than inhalers. Many nebulizers are not easy to carry around,3 but some new ones have been made to carry with you.3,4 You probably use one or more of these inhalers or nebulizers to take your COPD medicines. This piece will focus on the non-nebulized inhalers.
There are two common steps to correctly use your inhaler:5-9
- Preparing your inhaler for use (priming): This is done before using the first dose from your inhaler or when the inhaler has not been used for three to five days. Depending on the inhaler type, this step can include placing the medicine canister or cartridge in the pMDI or the SMI, shaking your pMDI a few times, and pressing the canister or the button on your pMDI or SMI for three or four test sprays away from your face. There is no need to prime the DPI and you should not shake a DPI.
- Regular inhaler use: These steps are performed every time you use your inhaler. Again, depending on your inhaler type, these steps may involve removing the mouthpiece cover or cap, pressing the canister to release the medicine from your pMDI, or turning the base of the SMI. Some DPIs already have the medicine loaded inside, meaning that you just have to open them, breathe out away from the inhaler, and then inhale rapidly and deeply.3,5,9 For other types of DPIs, you have to open the cap and mouthpiece, place a capsule inside it, pierce the capsule and then inhale.3,6 The capsule for an inhaler should never be swallowed like a pill.
A spacer should be used with pMDIs to help the medicine reach your lungs, especially if you find it hard pressing the canister or button and inhaling at the same time.10 The spacer can also help prevent you from getting oral thrush if you are taking an inhaled corticosteroid (ICS) with the pMDI.10
Please see the figure below to understand features of some commonly used inhalers.
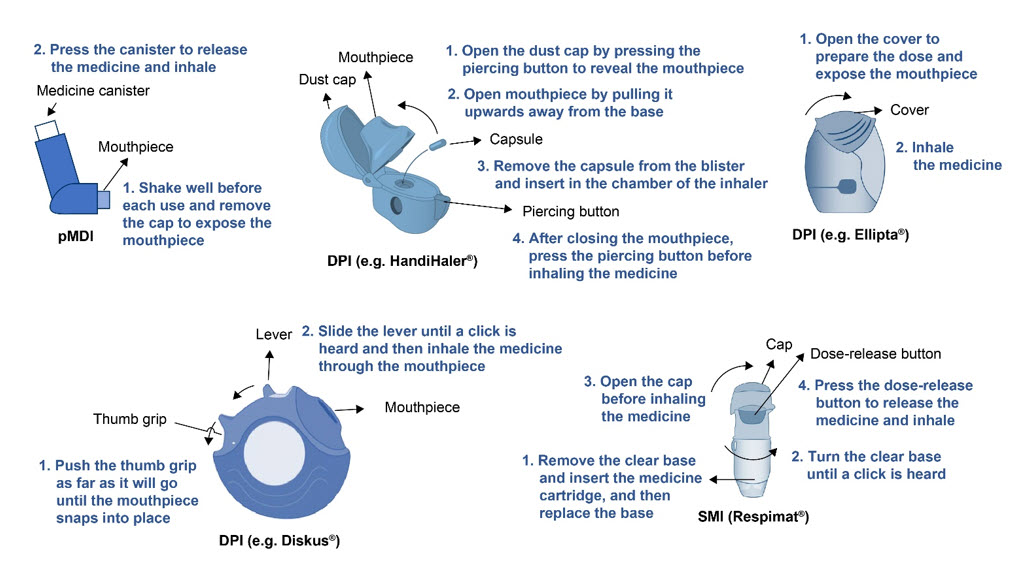
Figure. Features and steps for use for some commonly used inhalers.5-9
Make sure you read the instructions for use carefully before using your inhaler.
A number of errors may occur with inhaler use. Commonly reported errors include:11,12
- Not breathing out fully before inhaling the drug.
- Waiting too long to breath in through the inhaler or the spacer after pressing the canister on the pMDI or the button on the SMI.
- Not holding your breath for five to ten seconds after breathing in the medicine.
- Breathing in too fast or too slow—DPIs need rapid deep breaths in and pMDIs need slow deep breaths in for best results. Some people with COPD may not have the ability to breathe in fast and deep while using a DPI.13 If you have concerns, make sure you talk to your doctor or pharmacist who can advise you on correct inhaler technique.
Using the inhaler properly can be hard. Download the COPD Foundation app (COPD Pocket Consultant Guide – Patient View) for free from the Apple app store or Google Play and watch videos on how to use your specific type of inhaler.14 You can also ask your pharmacist to show you how to prime and use the inhaler. Be sure to show your doctor, nurse, or pharmacist your inhaler technique regularly to make sure that you are doing it right and getting the most from your medicines.
What is treatment adherence?
If you are taking your medicines, including your inhalers, regularly as agreed between you and your doctor, it means that you are adherent to your medicines and doing the best you can to get the most from your medicines. Adherence is important to make sure your medicines work for you. However, not being able to take all your medicines all the time is common in COPD.15 There are two types of non-adherence—intentional (when it is done on purpose) and unintentional (when it is not done on purpose).16 One of the most common causes of intentional non-adherence is the belief that the medicine is not helping you or that you do not need it all the time16 —and only when you are having more symptoms. It is important to talk to your doctor about which medicines are used every day (maintenance inhalers) and which medicines are used as-needed (reliever inhalers). Another common reason for intentional non-adherence is having trouble paying for all of the medicines.16 You need to talk to your doctor about these issues. Unintentional non-adherence may occur when you forget to take your medicines, do not know when or why you are taking your medicines, or when you have too many medicines.16 Talk to your doctor or nurse about using medicine reminders and see if you can get a different inhaler that combines two, or even three of your medicines, in one inhaler.
What factors influence treatment adherence?
Several factors can affect your ability to take all the medicines you and your doctor have agreed on, including:
- Being OK with or liking your inhaler: Being happy with your inhalers means that you are more likely to use them and should have less trouble breathing, and therefore be able to be more active and do what you want.17
- Having too many medicines and inhalers: You are more likely to forget your medicines or not use your medicines regularly and on time if you have several types of inhalers, or have to use them at different times of the day or several times a day.18,19 Remember to ask your doctor if it is possible to get two or three types of your COPD medicine in one inhaler.
- Feeling or believing that the medicine is working: Knowing that the medicine or inhaler is safe and effective means you are more likely to use it.20
- Social or family support: Having support or help from caregivers, friends, or family will also help you to take your medicines regularly.21
- Other medical conditions: Having depression22 or memory problems23 can make it harder to want to take or remember to take your medicines. Asking for help or support from others if you have other health problems is important.
What happens when you don’t take your medicines regularly and what can you do to take them regularly?
Not taking your medicine regularly can mean you have more symptoms, such as being short of breath, which may result in you not being able to do the things you would like to, and even ending up in the hospital.24 This can also increase the cost of taking care of your COPD.24
Using inhalers correctly takes practice. Ask your doctor, nurse, or pharmacist to teach you how to use your inhaler and then ask them to watch how you then use each of your inhalers. Set up reminders on your phone or a calendar and ask others with COPD how they remember to take their medicines. One place to talk with other people with COPD is on the COPD Foundation’s COPD360social community. Log in and join the online conversations. In addition to the resources of the COPD Foundation, your pharmacist can give you more information on COPD medicines and how to use them. Pharmacists can work closely with your doctor and talking to them can help you better care for yourself and your COPD.25
Acknowledgments
The authors meet the criteria for authorship recommended by the International Committee of Medical Journal Editors. The authors received no direct compensation for the development of this article. Writing, editorial support, and formatting assistance was provided by Praveen Kaul, PhD, and Frances Gambling, BA (Hons), of Cactus Communications, which was contracted and compensated by Boehringer Ingelheim Pharmaceuticals, Inc., (BIPI) for these services. BIPI was given the opportunity to review the article for medical and scientific accuracy as well as intellectual property considerations.
Disclosures
Dr. Yawn reports personal fees from Boehringer Ingelheim, AstraZeneca, GlaxoSmithKline, and Midmark, and grants from the COPD Foundation, Boehringer Ingelheim, and the National Heart, Lung, and Blood Institute (NHLBI) outside the submitted work.
Dr. Drummond reports grants from the NHLBI, the U.S. Department of Defense, and Boehringer Ingelheim outside the submitted work. He also reports personal fees from Boehringer Ingelheim, GlaxoSmithKline, AstraZeneca, Mylan-Theravance, Novavax, Parion, Midmark, and Philips outside the submitted work.
Ms. Rubin reports personal fees from Novartis and the U.S. Department of Defense outside the submitted work. She is associated with the COPD Foundation as a State Captain, which is a non-paid position.
References
- Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018; 19:10.
- van der Palen J, Klein JJ, Kerkhoff AH, et al. Evaluation of the long-term effectiveness of three instruction modes for inhaling medicines. Patient Educ Couns. 1997; 32:S87-S95.
- Kaplan A, Price D. Matching inhaler devices with patients: the role of the primary care physician. Can Respir J. 2018; 2018:9473051.
- Dhand R. Intelligent nebulizers in the age of the Internet: The I-neb Adaptive Aerosol Delivery (AAD) system. J Aerosol Med Pulm Drug Deliv. 2010; 23 Suppl 1:iii-v.
- Breo® Ellipta® prescribing information. GlaxoSmithKline. 2017. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/204275s012lbl.pdf. Accessed: November 20, 2019.
- Spiriva® HandiHaler® prescribing information. Boehringer Ingelheim Pharmaceuticals, Inc. 2009. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/021395s029lbl.pdf Accessed: November 20, 2019.
- Proventil® HFA prescribing information. Schering-Plough. 2009. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020503s039lbl.pdf Accessed: November 20, 2019.
- Stiolto® Respimat® prescribing information. Boehringer Ingelheim Pharmaceuticals, Inc. 2019. Retrieved from https://docs.boehringer-ingelheim.com/Prescribing%20Information/PIs/Stiolto%20Respimat/stiolto.pdf Accessed: November 20, 2019.
- Advair® Diskus® prescribing information. GlaxoSmithKline. 2008. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/021077s029lbl.pdf. Accessed: November 20, 2019
- Vincken W, Levy ML, Scullion J, et al. Spacer devices for inhaled therapy: why use them, and how? ERJ Open Res. 2018; 4.
- Sanchis J, Gich I, Pedersen S, (ADMIT) ADMIT. Systematic review of errors in inhaler use: has patient technique improved over time? Chest. 2016; 150:394-406.
- Lindh A, Theander K, Arne M, et al. Errors in inhaler use related to devices and to inhalation technique among patients with chronic obstructive pulmonary disease in primary health care. Nurs Open. 2019; 6:1519-27.
- Duarte AG, Tung L, Zhang W, et al. Spirometry measurement of peak inspiratory flow identifies suboptimal use of dry powder inhalers in ambulatory patients with COPD. Chronic Obstr Pulm Dis. 2019; 6:246-55.
- Thomashow B, Crapo JD, Drummond MB, et al. Introducing the new COPD pocket consultant guide app: can a digital approach improve care? A statement of the COPD Foundation. Chronic Obstr Pulm Dis. 2019; 6:210-20.
- Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008; 63:831-8.
- George M. Adherence in asthma and COPD: new strategies for an old problem. Respir Care. 2018; 63:818-31.
- Chrystyn H, Small M, Milligan G, et al. Impact of patients' satisfaction with their inhalers on treatment compliance and health status in COPD. Respir Med. 2014; 108:358-65.
- Toy EL, Beaulieu NU, McHale JM, et al. Treatment of COPD: relationships between daily dosing frequency, adherence, resource use, and costs. Respir Med. 2011; 105:435-41.
- Yu AP, Guérin A, Ponce de Leon D, et al. Therapy persistence and adherence in patients with chronic obstructive pulmonary disease: multiple versus single long-acting maintenance inhalers. J Med Econ. 2011; 14:486-96.
- Wiśniewski D, Porzezińska M, Gruchała-Niedoszytko M, et al. Factors influencing adherence to treatment in COPD patients and its relationship with disease exacerbations. Pneumonol Alergol Pol. 2014; 82:96-104.
- Trivedi RB, Bryson CL, Udris E, Au DH. The influence of informal caregivers on adherence in COPD patients. Ann Behav Med. 2012; 44:66-72.
- Khdour MR, Hawwa AF, Kidney JC, et al. Potential risk factors for medication non-adherence in patients with chronic obstructive pulmonary disease (COPD). Eur J Clin Pharmacol. 2012; 68:1365-73.
- Turan O, Turan PA, Mirici A. Parameters affecting inhalation therapy adherence in elderly patients with chronic obstructive lung disease and asthma. Geriatr Gerontol Int. 2017; 17:999-1005.
- Sanduzzi A, Balbo P, Candoli P, et al. COPD: adherence to therapy. Multidiscip Respir Med. 2014; 9:60.
- Xin C, Xia Z, Jiang C, et al. The impact of pharmacist-managed clinic on medication adherence and health-related quality of life in patients with COPD: a randomized controlled study. Patient Prefer Adherence. 2016; 10:1197-203.