
Stephanie Williams is a Registered Respiratory Therapist who enjoys educating, informing, and empowering people living with COPD and their families. As the Director of Community Programs, she is engaged with patients, caregivers, and healthcare professionals to improve the understanding and awareness of COPD.
For newly diagnosed patients with chronic obstructive pulmonary disease (COPD), it can be a scary and overwhelming time. At the COPD Foundation, we want to provide you with the most up to date and accurate information about your diagnosis. We asked our 360social community to share with us some common myths about COPD they have heard, so we could address these in a blog series.
Myth #1 - “If you are diagnosed with end-stage COPD you only have a short time to live”
Medicine has done a disservice to people living with COPD by labeling people as being ‘end stage’. Saying this about someone makes them feel as if their life is over or that they are moving full speed toward their death.
The fact is, when people are given a diagnosis of COPD, whether the words ‘end stage’ are mentioned or not, they often feel that their life will never be the same.
Remember how you felt when you were told you have COPD? What did that feel like? Overwhelming? Did you feel like you were in for the fight of your life? Like it wasn’t worth fighting? Depressed? Anxious?
All these feelings are normal, and when we have people newly diagnosed on 360Social, or are talking to their family members, we must remember what that felt like.
Just on COPD360Social alone, we have dozens of people who have been told they are ‘end stage’ who have been living productive lives for many years.
It is true that COPD progresses faster in some people than in others, but being proactive about your health, getting exercise, taking medications as prescribed, and avoiding triggers all play a big part in maintaining good health and quality of life. In summary – end stage is a terrible misnomer. Don’t let it get in the way of doing the things to keep you on the right track.
Myth #2 - “Patients on oxygen can become addicted and dependent on it”
It is likely that if you are prescribed oxygen, your tendency will be to try and limit your use or try to avoid using it so that you “don’t get addicted” to it.
The truth is that every living person on this planet is “addicted”, but people who have been prescribed supplemental oxygen just need it at a higher level than others.
A true addiction is like this: when you do something that makes you “feel good”, a chemical called dopamine is released in your brain. This part of your brain is called your “reward center” because when you do something like that, the dopamine levels make you feel good. This reward system also makes you crave the item, drug or activity.
Using supplemental oxygen does not affect the reward center in any way. There is no rush of dopamine to make your body crave it in the way you might crave nicotine or caffeine. It just isn’t that way.
Using supplemental oxygen simply increases the available oxygen that you are breathing in, making the oxygen molecules easier for the lungs to breathe in and making it easier for the blood to pick up and transport.
Not using oxygen as prescribed can put extra burden on the heart – making it work harder to meet the oxygen needs of the body. It makes it hard on the brain, too – since it needs oxygen to think clearly, keep up energy levels, and keep body systems functioning well.
Myth #3 – “The damage has already been done to my lungs from smoking, so why bother quitting” And another related myth - “If you stop smoking, COPD is gone.”
This is a common misconception. Smoking Cessation is very important.
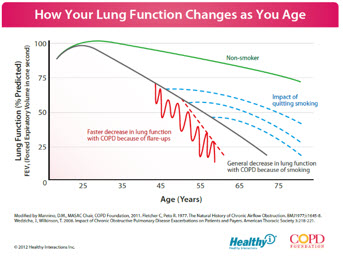
There is research that shows how continued smoking causes the lungs to worsen faster than if the person quits smoking. Part of the problem is that the smoking will cause more frequent exacerbations earlier than they would normally occur. With every exacerbation, the lung function decreases a bit. The worse the exacerbation, the more the decrease. The person’s ‘normal’ or baseline gets set lower each time. It is important for all smokers to stop smoking – even if there are no signs or symptoms, but it is critical for COPD patients to quit.
Along these lines – even if a person quits smoking, the damage is done. Further damage to the lung tissue can be prevented, but it doesn’t ever heal itself.
Another thing is that smoking makes it harder for your body to heal. Nicotine is a vasoconstrictor, or an agent that makes the blood vessels narrower and it keeps nutrients from being readily available to the skin. Have you ever noticed the skin of a long-time smoker? There is often wrinkling, dry skin, etc.
This same vasoconstriction limits the availability of white blood cells and other necessary components to heal cuts, or incisions, or even broken bones.
So, you can see that smoking affects more than just your lungs. Quitting smoking can have health benefits throughout your whole body.
There are lots of great tools out there to help you quit- and lots of people on 360Social who can share their tips and tricks to help you quit.
Need help quitting? Check out Quitline, a tobacco cessation service available through a toll-free telephone number. Quitline’s are staffed by counselors trained specifically to help smokers quit. Quitline: 1-800-QUIT-NOW (1-800-784-8669)