*Please click on the images below to see larger versions
The COPD Foundation is excited to announce the launch of an updated version of the COPD Pocket Consultant Guide (PCG) app for health care providers! The app, designed to support the treatment and management of COPD, is available for both iOS and Android. The latest version contains an updated therapy chart, including the latest medications, inhaler and nebulizer instruction videos, depression and anxiety screeners, a pulmonary referral checklist, the CAPTURE tool, and much more.
In addition, users can toggle between this track and one specifically for patients and caregivers by clicking on “Change View” in the upper right of the main menu screen. The patient and caregiver track has several exciting features, including an interactive "Goal Setting/For My Next Visit" tool, inhaler and exercise videos, activity tracking, a medication and immunization wallet card, and more. We hope you will share this with your patients.
Learn more about the health care provider track below.
Guidance on Using the Provider Track of the App
Main Menu
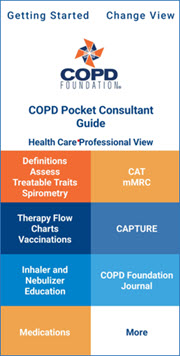
Definitions/Assess Treatable Traits/Spirometry
On the main menu, if the Definitions/Assess Treatable Traits/Spirometry header is selected, the user will access information on the definition of COPD, traits associated with COPD that may have therapeutic implications for your patients, and spirometry grade definitions. If you enter your patient's spirometry testing results into the interactive tool, you will be brought to the spirometry grades section, which includes information from GOLD (Global Initiative for Chronic Obstructive Lung Disease).
The CAT and MMRC
On the main menu, if you select the CAT/MMRC, it will trigger an interactive model. These tools can be used to assess your patient's COPD symptoms. After your patient answers each question, a score is calculated. A pop-up screen will then appear, explaining the patient's results and offering treatment guidance.
CAPTURE
The CAPTURE tool can be found on the main menu. This screening tool is used to help find patients who are at risk for COPD. After your patient answers each question, your patient's COPD risk is calculated. The assessment results will indicate if further testing, such as spirometry, is suggested.
Additional Features and Resources
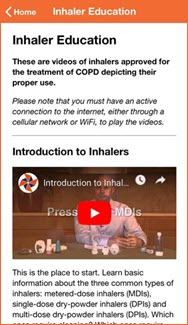
Inhaler Education: This takes the user to videos of all available inhaler devices. Note: if you are unable to hear sound on the videos, ensure that your phone or table is not on soft mute. On the iPhone, there is a switch on the left side of the phone that switches the ringer to mute or silent. If the phone or tablet is flat, the switch should be down.
Exacerbations: This page provides definitions and potential therapy options.
Therapy Flowchart: This flowchart provides the most recent updated versions of the pathways as they appear on the new version of the Pocket Consultant Guide for developing a treatment approach to COPD and ACO.
Medications: This page provides a listing of FDA-approved medications and dosing. By pressing either "Non Brand" or "Brand", you can switch the screen between trade and generic drug names.
Clicking on the "More" box will take you to a number of other options outlined below.
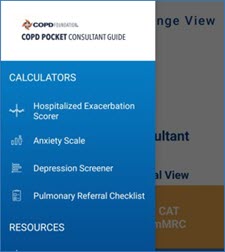
From the main menu, if you click on “More”, you will be brought to a secondary menu. Here you will find:
1) The exacerbation scorer DECAF, which predicts mortality risk for those hospitalized with an exacerbation.
2) The GAD-7, an anxiety scorer.
3) The PHQ-9, a depression scorer.
4) A mnemonic called HELP OUT to suggest when to consider referring to a pulmonologist.
5) And more!
In the Resources section, we provide information on exacerbation definitions and potential therapy options, the Fletcher-Peto Impact of Smoking graph, information on the NHLBI COPD National Action Plan, and links to the My COPD Action Plan, the COPD Foundation's Pocket Consultant Guide, and the COPD Foundation Guides for Better Living.
Tips
- Several pages are printable. Click on the printer icon to print a particular page.
- To return to the main menu, click on the house icon in the upper right corner of the page.
Supported Mobile Devices
Please note that the COPD Pocket Patient Guide is intended for Android devices running Android 9 and up, and iPhones and iPads with iOS 16.0 or later.
For comments on the structure or function of the app, please contact the COPD Foundation Education Team at edteam@copdfoundation.org.
Learn more about our Patient & Caregiver Track
Please spread the word. We are trying to make a difference.